If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Ovarian cancer
Key points about ovarian cancer
- Ovarian cancer is a type of cancer that affects the ovaries (affecting anyone born with female reproductive organs).
- It's one of the most common types of cancer in women over the age of 50 years and is usually diagnosed when it's already advanced.
- If you have ongoing abdominal or back pain, abnormal vaginal bleeding, nausea or bloating, see your healthcare provider for a check-up.

The ovaries are part of the female reproductive system. They produce ova (eggs) and release certain hormones, such as oestrogen and progesterone.
Ovarian cancer is when cells within the ovaries grow abnormally and multiply rapidly. These cells are known as cancerous or malignant cells and the growth is known as a tumour or mass. Ovarian cancer is more common as you get older, but it also runs in families and can affect young women too.
There are 3 main types of ovarian cancer.
Video: What is ovarian cancer?
This video may take a few moments to load.
(Dr Sarah Jarvis, Patient Info, UK, 2018)
There are 3 main types of ovarian cancer (and many other subtypes). The treatment and chance of cure will be different for each type of cancer and will depend on how far the cancer has spread.
- Epithelial cancers start from the cells that line the outside of the ovaries. This is the most common type of cancer and causes about 90% of all ovarian cancers. It usually occurs after menopause.
- Germ cell cancers start from the cells that produce the eggs. This is the second most common type of ovarian cancers and usually occurs in the 20–30-year-old age group.
- Stromal cancers arise from the tissue that makes hormones and supports the ovary. These are quite rare.
There are also cancers that originate from the lining of the pelvic cavity or from the fallopian tubes (tubes connecting the ovaries to the womb). As they are closely related to the ovaries, they are sometimes included when describing ovarian cancers.
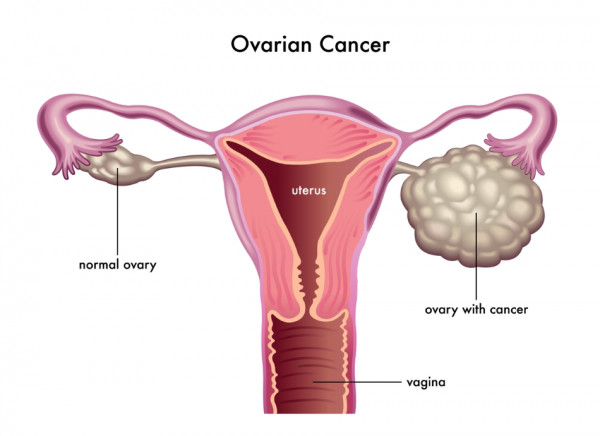
Image credit: Depositphotos
In the image above, the right ovary (left side of picture) is normal (about the size of a walnut), the left ovary (right side of picture) is much bigger and has an ovarian cancer.
Ovarian cancer doesn't usually cause any obvious symptoms until the cancer is quite advanced. Some of the symptoms of ovarian cancer are:
- Indigestion, persistent bloating and nausea (feeling sick).
- An increase in waist size.
- A loss of appetite or feeling full early.
- Unexplained weight loss.
- A persistent pressure in the lower back or pelvis.
- A change in bladder or bowel habit.
- Feeling tired or a lack of energy.
- Postmenopausal bleeding.
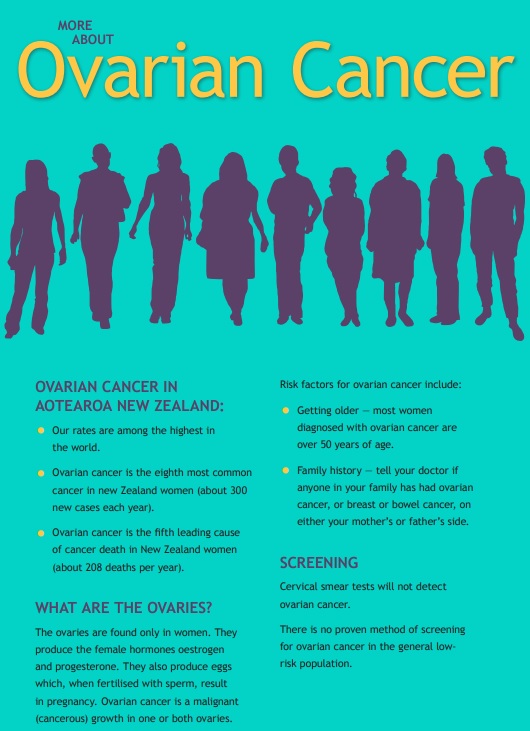
Most ovarian cancer occurs in women after menopause. The average age to be diagnosed is 65 years old. Ovarian cancer is slightly more common in Māori and Pacific Peoples.
- Examination: Your healthcare provider will need to perform a gentle pelvic and abdominal examination to feel for any masses or anything abnormal.
- Ultrasound: An ultrasound is usually the first step in making a diagnosis. Most ovarian masses can be seen with ultrasound. In order to be able to see the ovaries, a transvaginal ultrasound will be performed. This uses a slim ultrasound probe placed inside your vagina to see the pelvic organs clearly. The sonographer performing the scan will discuss this with you before the procedure.
- CT scan: A CT scan is another type of imaging used to see ovarian cancer. It's sometimes used after an ultrasound scan or in combination with other types of scans to help with staging (working out how advanced the cancer is).
- Blood tests: Your healthcare provider will arrange for a number of blood tests, but one important test is called the Ca-125. This measures a protein in the blood that is often increased when a woman has ovarian cancer (in about 80% of cases). This protein can also be increased for other reasons (eg, endometriosis or a ruptured ovarian cyst) so an increased level doesn't always mean there is cancer, especially if a woman is still having periods. The test needs to be interpreted along with the other information.
Screening means testing women to see if they have cancer, when they aren’t having any symptoms. For a screening test to be effective, it needs to be safe, relatively easy and not too expensive. It also needs to be able to find cancers at an earlier stage, and improve the outcomes for these people.
If a screening test is positive, then it's usually followed up by further tests or procedures to confirm if a cancer is present (there are often multiple causes of a positive screening test). This can cause a lot of worry, and can result in unnecessary procedures or operations for people who don’t have cancer.
At the moment, there are no screening tests that are recommended for ovarian cancer. The tests we have available do not reliably detect early ovarian cancers or significantly change the outcome for these women. So it's important to know about ovarian cancer and which symptoms to look out for, and to see your healthcare provider if you're concerned.
Genetic and inherited ovarian cancer
Women who have a family history of breast or ovarian cancer may have a higher risk of cancer themselves. Some of these women will carry a genetic abnormality called BRCA1 or BRCA2, or another type of cancer gene (which is more rare). These genes increase a woman’s risk of breast cancer, bowel cancer and ovarian cancer. If a woman (or a man) is found to have a BRCA gene mutation they may also pass this on to their children.
Finding out that you have a high risk of developing cancer is a life-changing event, so it's important to have all the right information before the test is performed. If you have lots of cancer in your family (particularly breast and ovarian cancer), please discuss this with your healthcare provider.
Genetic screening for BRCA (and other cancer genes) is a lengthy and expensive process, so there are specific criteria required before testing is recommended.
Women with the BRCA genes are recommended to have their ovaries and fallopian tubes removed after they have completed their families. This reduces ovarian cancer by at least 90%. Yearly screening of women without symptoms (with a blood test or pelvic ultrasound) is not recommended, because it doesn’t reliably find early ovarian cancer or change the outcome.
Read more about the BRCA gene.
Treatment for ovarian cancer will depend on the type of cancer you have and the stage it is (how much it has spread). Treatment may involve a combination of surgery (to remove as much of the cancer as possible) and chemotherapy (to kill the remaining cancerous cells). Some people also choose to use complementary therapies. Palliative care is also available (specialised medical care to optimize your quality of life), and may be recommended if the cancer is very advanced.
Treatment options
Surgery
Most women with ovarian cancer will have surgery to remove as much of the cancer as possible. In germ cell tumours or in early stage ovarian cancer (stage 1), it may be possible to just remove the ovary. However, as the cancer can spread easily from the ovary to the uterus, fallopian tubes and omentum (membrane covering the organs in the abdomen and pelvis), often these organs are removed during the first surgery as well.
Surgery will not only treat the cancer by removing as much as possible, but it's also done to see if the cancer has spread. This is called staging.
Sometimes the cancer is too advanced for surgery to be possible. In this case, chemotherapy may be recommended as the first-line treatment.
Chemotherapy
Most women are also referred to a medical oncologist to discuss chemotherapy options. Even if all of the visible cancer has been removed, it is likely there are still cancer cells present (which are too small to be seen by the naked eye). Chemotherapy aims to kill these cells or shrink remaining masses, to prolong the time before the cancer grows again or causes symptoms. In a small number of women, chemotherapy can kill the cancer cells and prevent them from coming back (cure cancer).
Chemotherapy is usually given as a combination of different drugs. This improves the chances of killing the cancer cells but may also increase the damage to normal cells. Your specialists will recommend the best treatment for you and discuss these options with you.
Side effects of chemotherapy
Because the aim of chemotherapy is to kill cancer cells, these treatments may also damage normal cells. Cells that are rapidly dividing (eg, skin, hair and cells from the intestines) are particularly at risk of being damaged. This can cause hair to fall out and can also cause significant tiredness, a loss of appetite, nausea (feeling sick) or diarrhoea (runny poo). The team looking after you can help with many of these symptoms, so it's important to let them know what's happening.
Complementary and alternative therapies
The team providing your care will primarily be trained using conventional medical therapies. Some people may wish to use other therapies as well. Remember that it's your right to choose whatever therapy or therapies you choose, but also remember that your team is trying to look after you using the best information and evidence available. Some complementary and alternative therapies (including herbal or dietary supplements) will interfere with the treatment you receive, although many alternative therapies can be used alongside standard medical treatment. So it’s important to tell your team about anything else you are taking or doing.
Palliative care
Everybody starts their treatment for cancer in the hope that they will be cured and be able to get back to a normal life. Unfortunately, that isn’t the case for everyone. The palliative care team is trained to provide the best possible care to you and your whānau, to optimise your quality of life and provide support. They may be involved early-on in your care, to assist in managing symptoms from chemotherapy/surgery, or later on in your care to support you towards the end of your life. Read more about palliative care.
Who is in my treatment team?
Modern treatment of cancer is a team effort. You may have a lot of different people for different teams looking after you, but you should always have 1 or 2 main people you can contact if problems arise. Some health professionals that you may see include:
- Surgeons – who undertake any necessary surgery.
- Oncologists – who see you in clinic and look after the administration of chemotherapy.
- Radiologists or radiographers – who undertake and interpret the ultrasounds and other scans.
- Specialist nurses – your treatment is often supervised by nurses specialised in giving chemotherapy.
- Support staff – these range from the receptionist you see when you arrive for an appointment, to the orderly who collects your treatment, to the pharmacist who will be involved in your care.
- Dietitians – who can advise on the best foods to eat when recovering from surgery or when having chemotherapy.
- Social workers – who are able to inform you of available support services – especially if you're not able to work.
Gynaecological Cancer Foundation Facebook page(external link)
Information and support for women affected by gynaecological cancers, including uterine, ovarian, cervical and vulval/vaginal cancers.
Cancer Society(external link)
The Cancer Society of New Zealand is the country’s largest source of information about cancer and its effects. This website provides information on types of cancer, diagnosis, methods of treatment and advice on living with cancer.
Look Good Feel Better(external link)
Free Feel Better Class for any cancer patient with any cancer.
Cure Our Ovarian Cancer(external link)
The Cure Our Ovarian Cancer is a New Zealand registered charity that locally raises awareness and advocates for women with ovarian cancer, and globally raises funds for research on a rarer subtype called low-grade serous cancer. Women can also find access to support groups and other information on the website.
Ovarian cancer(external link) Cancer Society, NZ
Ovarian cancer(external link) NHS Choices
Gynaecological Awareness(external link) Talk Peach, NZ
Ovarian cancer(external link) Talk Peach, NZ
Ovarian Cancer Foundation(external link) NZ, has resources and guides
Resources
Supporting someone with cancer [PDF, 3 MB] Cancer Society, NZ
Ovarian cancer(external link) Cancer Society NZ
References
- Ovarian cancer symptoms(external link) Community HealthPathways – Auckland Region, NZ
- Familial breast or ovarian cancer syndromes(external link) Community Health Pathways – Auckland Region, NZ
- Ovarian cancer(external link) Te Aho o Te Kahu Cancer Control Agency, NZ
- Ovarian cancer a patient's guide(external link) Family Doctor, NZ
- Ovarian cancer – recognition and initial management(external link) NICE guidelines, UK
- Ovarian cancer – early detection and referral(external link) BPAC, NZ, 2023
Ovarian cancer(external link) B-QuiCK BPAC, NZ
Brochures
Cancer Society NZ, 2019
Cancer Society, NZ, 2015
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Phoebe Hunt, Sexual Health Registrar, Northland
Last reviewed:
Page last updated:





