Muscular dystrophy
Key points about muscular dystrophy
- Muscular dystrophy (MD) refers to a group of conditions that cause muscle weakness that gets worse over time.
- It's caused by changes (mutations) in genes that you inherit from your parents.
- The different types of MD vary in terms of when symptoms develop, which muscles they affect and how severe they are.
- Life expectancy can vary depending on the type of MD.
- There's no cure for MD, but there is treatment and support to help you manage your condition.

MD refers to a group of inherited conditions that gradually cause your muscles to weaken. The muscle weakness gets worse over time, resulting in increasing disability.
There are several different types of MD which vary in age of onset (when it starts), severity (how bad it is) and the groups of muscles it affects. Duchenne muscular dystrophy (DMD) is the most common type of MD.
As MD progresses, breathing and heart problems can occur. Not all types of MD cause severe disability and many don’t affect how long you’ll live.
In most cases, MD runs in families. This means it occurs because you have inherited a faulty gene (a gene mutation) from one or both of your parents. Occasionally, a new gene mutation can occur in someone with no family history of MD.
The changes occur in genes that are responsible for healthy muscle structure and function, meaning that your muscles can't work properly.
With Duchenne muscular dystrophy (DMD), the most common form of MD, the gene mutation is on the X-chromosome so boys inherit the gene from their mother.
The main symptom of MD is muscle weakness which gets worse over time. Different types of MD affect different muscle groups in your body. The muscle weakness may be mild, moderate or severe and may progress slowly or quickly depending on the type of MD.
Symptoms can start anywhere between birth and middle age, depending on the type of MD. In babies, the muscle weakness may be noticed as floppiness. In older babies and young children, the weakness may show up as a delay in learning to hold up their head, sit up, crawl or walk.
Other symptoms include:
- muscle wasting – your muscles become thin
- muscle hypertrophy – bulkier than normal muscles, even though they work less well
- aches or pains in your muscles
- contractures – tight joints, due to tightness of your muscles or reduced movement of your joints
- symptoms of heart disease (sometimes without much muscle weakness).
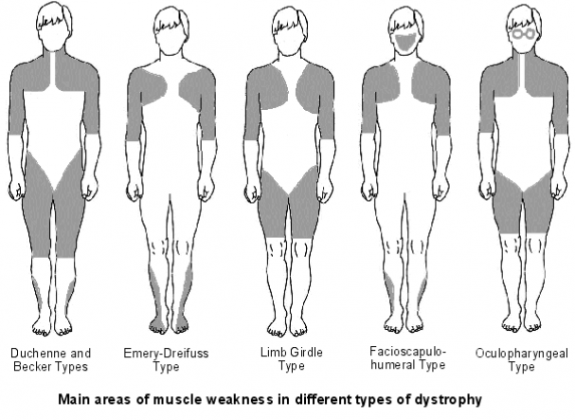
Image credit: Mantas1234512345 via Wikimedia Commons
There are several types of MD that are grouped according to:
- the extent and pattern of muscle weakness
- the age when it starts
- how quickly it progresses
- the severity of symptoms.
Duchenne muscular dystrophy (DMD)
This is the most common form of MD. It typically starts to be seen between 1 and 3 years of age and mostly affects boys.
Symptoms include:
- delay in reaching motor milestones, such as sitting and standing on their own
- difficulty standing, walking, running, jumping
- a waddling gait
- walking on their toes
- large calf (lower leg) muscles
- frequent falls and clumsiness.
A wheelchair may be needed in childhood as walking becomes more and more difficult, and scoliosis (sideways curve of the spine) may develop. The child may also have learning disabilities.
Life expectancy has improved due to advances in treatment and care with many people surviving into their 20s or 30s, and there are cases of men living into their 40s or 50s. Most people with DMD die from heart or respiratory failure.
Myotonic dystrophy (known as DM because the Latin name is Dystrophia Myotonica)
This is the most common adult form of MD. It can start at any age, usually between 20 and 30 years of age, but can be seen in babies. It often progresses slowly.
Symptoms include:
- myotonia (muscle stiffness) which is when the muscles are slow to relax after contraction – it only occurs in this type of MD and the face, jaw, and neck muscles are often affected first
- weakness in different muscles, particularly the face
- cataracts (when the lens of your eye becomes cloudy) can develop
- slow heart arrhythmias (irregular heartbeats).
Many people with DM have normal life expectancy, except for those with the severe congenital form. DM can cause problems with anaesthesia and childbirth.
There are different forms of DM. DM type 1 (DM1) affects the muscles further away from the centre of your body first and can affect other body systems including your heart, adrenal glands, thyroid, eyes and gut. DM type 2 (DM2) affects bigger muscles closer to the centre of your body. It has fewer other systems involved, and is typically less severe.
Facioscapulohumeral muscular dystrophy disease (FSHD)
This affects people from childhood through to adulthood and progresses slowly. Symptoms in children include being unable to squeeze their eyes tightly shut, meaning they sleep with their eyes slightly open. They also can’t purse their lips (to blow up a balloon). In teens and adults, it affects the muscles of the face (unable to pucker lips to whistle, crooked smile) and shoulders, upper arms, lower legs and upper back. The muscle weakness is asymmetric, it affects each side of the body differently.
Life expectancy isn’t usually affected but some people will need to use a wheelchair (10 to 20%) and breathing problems may develop.
Becker muscular dystrophy (BMD)
BMD can develop from childhood to early 20s and boys are more likely to be affected. It's similar to DMD but is less severe and progresses more slowly.
Children may be slow to walk and early symptoms include walking on their toes, having frequent falls and finding it hard to get up off the floor.
People with BMD often have a normal lifespan but are at risk of heart and breathing problems and may need to use a wheelchair in later life.
Limb girdle muscular dystrophy (LGMD)
LGMD usually develops somewhere in late childhood to early adulthood.
Symptoms can include:
- weakness and loss of muscle mass around shoulders, hips, thighs and arms
- difficulty lifting things, running, climbing stairs and getting up from low seating
- a waddling gait (way of walking)
- heart and breathing problems.
There are many differently types of LGMD and how it progresses depends on the type. Generally, the earlier the symptoms emerge, the faster the condition progresses. Some people may have little disability and other may lose the ability to walk.
Oculopharyngeal muscular dystrophy
This type develops when people are in their 40s and 50s. It affects the muscles in your eyes and throat resulting in droopy eyelids and difficulty swallowing food.
People with oculopharyngeal MD are at risk of chest infections because of food getting into their lungs. Their limbs may be affected later in life and some people will become unable to walk. It doesn’t usually affect life expectancy.
Emery-Dreifuss muscular dystrophy (EDMD)
This mainly affects boys in their childhood or teenage years. It involves muscle contractures (shortening of muscles or tendons around joints) which limit range of movement – especially of arms, neck and feet. People with EDMD may often trip over things and may have difficulty with:
- straightening their elbows or bending their neck forward
- difficulty lifting heavy objects
- raising their arms above their head.
EDMD usually progresses slowly, but life expectancy may be limited because of the risk of heart problems from having a slower and irregular heartbeat. A wheelchair may be needed in later life.
Congenital muscular dystrophy (CMD)
CMD is either present at birth or symptoms develop before 2 years of age. Children with CMD are generally late to reach their developmental milestones related to movement and muscle control. They're unable to sit or stand without support and have poor head control and weak muscles – sometimes called ‘floppy baby’.
It can cause mild to severe disability. People with CMD may develop contractures (shortened muscles or tendons around joints), scoliosis (curved spine), and breathing and swallowing problems. It can also affect your nervous system leading to speech and vision problems and seizures. Cognitive development may be affected.
It doesn’t always progress and some tamariki with CMD may have a normal lifespan.
Manifesting carriers of DMD or BMD
Usually females who carry the affected gene pass on the disease but are unaffected themselves. A manifesting carrier is a female who carries the affected gene and also has symptoms of DMD or BMD, which usually only affect males.
This can occur with no known family history of BMD or DMD, so all females who are suspected of having any form of muscular dystrophy should be tested to see if they could be a manifesting carrier because of the genetic implications for other whānau members.
Manifesting carriers may have heart problems that cause shortness of breath, or be unable to do moderate exercise. If untreated, these heart problems can be quite serious, and even life-threatening.
Read more about the different types of MD(external link).
MD is diagnosed based on the specific presentation of muscle weakness and any other features. The pattern of weakness helps determine the type of MD. A diagnosis can generally be confirmed by genetic testing.
Other people in your whānau can also be tested to see if they have an MD gene.
Diagnosis will also involve some or all of the following:
- discussion of family history of MD
- blood tests (including creatine kinase – levels can be very high)
- electrical tests on your nerves and muscles
- muscle biopsy (where a small tissue sample is removed for testing).
MD can be difficult to diagnose because other disorders have similar symptoms, and some people have no findable genetic cause for it.
MD can't be cured so treatment aims to help you manage the condition and stay as independent as possible. It also aims to prevent complications of muscle weakness, reduced mobility and heart and breathing difficulties.
Each person experiences MD differently, so treatment will be tailored to individual’s needs and will involve a combination of approaches and healthcare providers.
Steroid medicines play an important part in the treatment of Duchenne MD (DMD), and have been shown to slow its progression. Children with DMD should begin steroid treatment before they start to lose motor skills.
Other treatments for MD include:
- medicines to treat effects such as muscle spasms, cardiomyopathy or arrhythmias
- physiotherapy to help you maintain muscle function – starting exercises and stretching early on can help keep your muscles flexible and strong
- occupational therapy to help you learn new ways of doing things, make adjustments to your immediate living area and provide you with equipment to assist you.
- respiratory therapy (eg, breathing exercises) to help with respiratory problems
- support aids (eg, splints, braces, or wheelchairs) to help with stability and mobility
- surgery to correct contractures or spinal curves or to implant a pacemaker to prevent heart problems
- speech-language therapy
- assisted ventilation, which you may need if MD affects your breathing muscles.
To prevent infections, it's important to be vaccinated for pneumonia and to keep up to date with influenza and COVID-19 vaccinations.
Some types of MD may mean that you’re at increased risk of heart problems, because of the weakening of your heart muscles. It's important that your heart function is assessed regularly once MD has been diagnosed.
Life expectancy varies depending on the type of MD. However, due to advances in treatment and care, people with MD now live longer. With the most common type of MD, Duchenne muscular dystrophy, survival into the early 30s is becoming more common, and there are cases of men living into their 40s and 50s.
You can get support for yourself and your family through counseling, joining Muscular Dystrophy New Zealand(external link), and talking to friends and whānau about your experience.
Exercise as much as you are able to. The health benefits can help you maintain your mobility, manage any pain and improve your general quality of life.
Get the recommended vaccinations(external link) for people with neuromuscular diseases, such as the annual flu, pneumococcal and COVID-19 vaccines.
Apps reviewed by Healthify
You may find it useful to look at some physiotherapy and exercise apps.
The Muscular Dystrophy Association NZ(external link) (MDANZ) offers educational, emotional, financial, personal and workplace assistance.
MDANZ has a free nationwide fieldworker service(external link) and can also arrange funding for counselling. Fieldworkers get to know your strengths, needs and goals and can help you access further support, services and resources as you need them.
There are regional branches and you can phone the national office on 0800 800 337.
There’s also a Kiwi Kids with DMD Facebook support group(external link).
Muscular dystrophies(external link) Muscular Dystrophy NZ
Muscular dystrophy(external link) NHS Choices, UK, 2015
Muscular dystrophies – an overview(external link) Patient Info, UK
Myotonic dystrophy(external link) Myotonic Dystrophy Foundation, NZ
Apps
Physiotherapy and exercise apps
References
- Muscular dystrophies – an overview(external link) Patient Info, UK, 2023
- Muscular dystrophies(external link) Muscular Dystrophy NZ
- Duchenne muscular dystrophy(external link) MDA, US
- Vaccination recommendations(external link) Muscular Dystrophy NZ
- Muscular dystrophy (external link) NHS, UK, 2021
- Muscular dystrophy(external link) NIDS, NIH, US
- Muscular dystrophy(external link) Mayo Clinic, US, 2022
Duchenne muscular dystrophy(external link) Patient Info Professional, UK, 2016
Beckers muscular dystrophy(external link) Patient Info Professional, UK, 2016
Facioscapulohumeral muscular dystrophy(external link) Patient Info Professional, UK, 2016
Limb girdle muscular dystrophy(external link) Patient Info Professional, UK, 2016
Neuromuscular conditions(external link) Goodfellow eLearning, 2019
Duchenne muscular dystrophy and steroid use(external link) NZ Paediatric Neurology Clinical Network, 2018
The standards of care for DMD(external link) were updated in 2018:
Part 1: Diagnosis, and neuromuscular, rehabilitation, endocrine, and gastrointestinal and nutritional managements(external link)
Part 2: Respiratory, cardiac, bone health, and orthopaedic management(external link)
Part 3: Primary care, emergency management, psychosocial care, and translations of care across the lifespan(external link)
The following 3 reviews were conducted on behalf of the Myotonic Dystrophy Foundation and were published in ‘Neurology Clinical Practice’, a publication of the American Academy of Neurology.
- Consensus-based care recommendation for adults with myotonic dystrophy type 1(external link) Myotonic Dystrophy Foundation, US, 2018
- Consensus-based care recommendation for adults with myotonic dystrophy type 2(external link) Myotonic Dystrophy Foundation, US, 2019
- Consensus-based care recommendation for congenital and childhood-onset myotonic dystrophy type 1(external link) Myotonic Dystrophy Foundation, US, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Erik Andersen, Paediatric Neurologist, Wellington
Last reviewed:





