There's no cure for Meniere's disease, but a combination of lifestyle changes and medication can help make attacks less severe – mainly helping with vertigo. There's no treatment for the hearing loss that happens with Meniere's disease.
Lifestyle changes
Meniere's disease can be hard to manage and tough to live with. Here are a few lifestyle changes that may help:
- Limit salt in your diet to less than 2,300 milligrams per day, and don’t have large amounts all at once. Follow a ‘no added salt’ diet – this means not adding salt to your food while you are cooking or before you eat, and avoiding foods which taste salty (use other herbs and spices to make your food tasty.) Food and drink high in salt can boost the amount of water in your inner ear.
- Limit caffeine and alcohol as they can trigger attacks for some people. Keeping a diary can help you work this out.
- If you smoke, quit. Smoking can increase attacks.
- Seek out a support group. Although there isn't an active support group dedicated to Meniere’s disease in Aotearoa New Zealand, there are online support groups in other countries.
During an attack
When you have an attack:
- Lie down and hold your head very still until the symptoms go away.
- Focus on a faraway object that isn't moving and notice the feeling of clothes and air against your skin – this helps your brain sort out the mixed balance messages it's getting.
- Don’t drive.
- Avoid watching TV, reading, bright lights or anything that makes your symptoms worse – keeping a diary may help you figure out what makes them worse.
- After an episode don’t rush back into movement – your body needs rest, and to slowly adjust to normal balance again.
Between attacks
When you have an attack of vertigo, you're at risk of falls and injury. Between episodes you can take steps to help protect yourself, such as:
- Do exercises to improve your balance. This is called vestibular physiotherapy. Your GP or nurse practitioner can refer you. This can reduce your risk of falling and hurting yourself or others.
- Make changes to reduce your risk of injury during a vertigo attack, eg, install grab bars in your bathroom.
- Wear shoes with low heels and non-slip soles.
Medicines
Your healthcare provider may prescribe medicines to take during an attack:
- Medicines that control nausea and vomiting during an episode of vertigo (called anti-nausea medications) such as prochloperazine, promethazine or cyclizine.
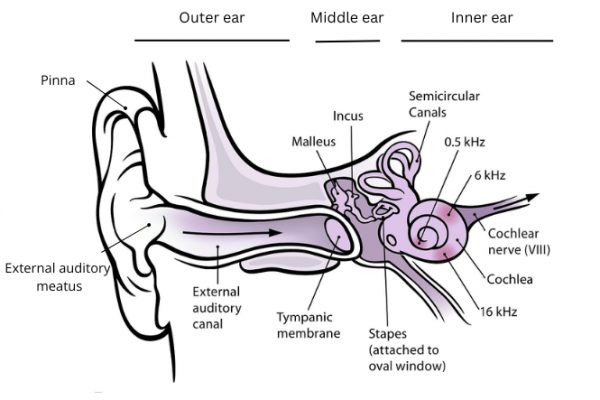
- Medicines to reduce inflammation in the inner ear, such as prednisone. You may be started on a high dose which is reduced slowly over a few days.
Your healthcare provider may prescribe daily medicine to prevent further episodes, eg, betahistine or bendroflumethiazide. It's not clear whether these medicines work well so your healthcare provider may discuss this with an ENT specialist.
Other treatments
Hearing aids for hearing loss
- If you develop permanent hearing loss, you may benefit from a hearing aid.
- If loud sounds become distressing then an audiologist or hearing therapist can provide you with advice on compression hearing aids which may help to ease this symptom.
Sound therapy for tinnitus
- If you develop permanent noises in the ear (tinnitus) then various strategies may be advised.
- For example, an audiologist or hearing therapist may advise on sound therapy.
- This often uses a CD or an MP3 player to play soothing and relaxing sounds, helping to distract you from the sound of tinnitus.
- Some people have found coping strategies, relaxation training, counselling, and other such techniques useful
Physiotherapy for loss of balance
- A physiotherapist may be involved if your balance becomes permanently affected (in severe cases).
Intratympanic gentamicin
- An injection through the eardrum can disable the pressure detectors in the inner ear. This is done by an ENT specialist.
Surgery
- Rarely, surgery is used to stop very severe symptoms. But this can cause complete deafness and has risks because it is so close to the brain.
Apps reviewed by Healthify
You may find it useful to look at some Tinnitus apps and Vertigo apps.