Lupus is a type of autoimmune condition. This mean that your body's immune system produces antibodies that attack healthy tissue as if it was a foreign body, such as bacteria or a virus.
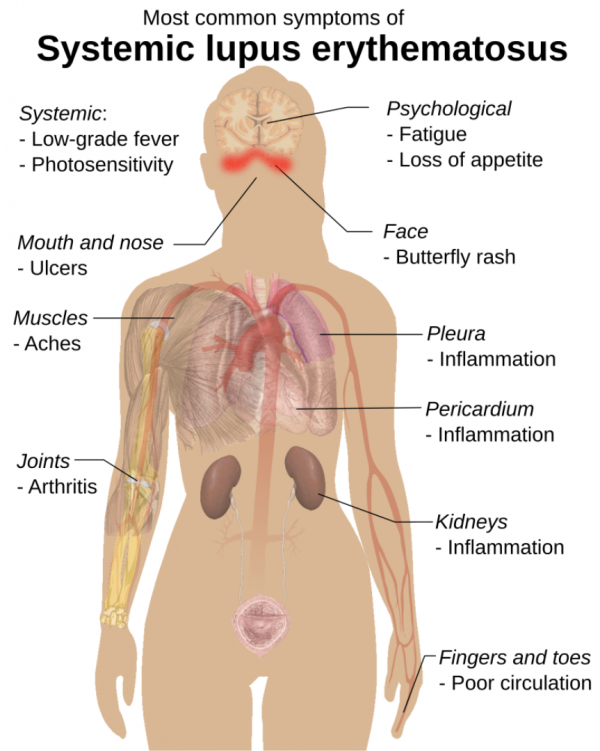
Lupus is a chronic (long-term) and complex condition that affects different people in different ways. It may affect joints and skin. It can also affect blood vessels and internal organs, such as your kidneys, brain, heart and lungs.
Approximately 1 in every 900 people in Aotearoa New Zealand is diagnosed with lupus. It's more common in Pacific Peoples, Māori and Asian people, and in other ethnic groups with darker skin. It can occur in men, women and children, but it's much more common in women and is usually diagnosed between the ages of 15 and 45.