Wishing everyone a safe and happy Christmas and New Year – Meri Kirihimete from the Healthify team.
Arthritis in children
This page is about juvenile idiopathic arthritis (JIA)
Key points about arthritis in children
- Learning that your child has arthritis can be confusing and worrying.
- You may have lots of questions, especially if reaching a diagnosis has taken some time, as it often does.
- JIA (juvenile idiopathic arthritis) is the most common type of arthritis in children and young people under 16 years of age. This page focuses on JIA.
- The good news is that with good management and support, your child can live a normal life.
- Some will outgrow the condition and will not need treatment as adults.

Juvenile idiopathic arthritis (JIA) is the name given to a number of types of arthritis that occur in children.
JIA is an autoimmune condition. This means that your body’s immune system, which normally protects against infection, attacks healthy tissues by mistake, creating inflammation. The symptoms of JIA vary from person to person and can come and go from day to day and week to week. Symptoms will be worse during occasional ‘flares’; at other times the condition seems to disappear for a time.
Joints are sore and swollen because in JIA, the immune system attacks the synovium, the thin membrane that lines the joints and makes a fluid that helps them move smoothly. If inflammation is not treated, it can damage, joints, cartilage and bones and weaken muscles around the joint.
The image below shows a joint with the synovial lining, tendon and cartilage labelled.
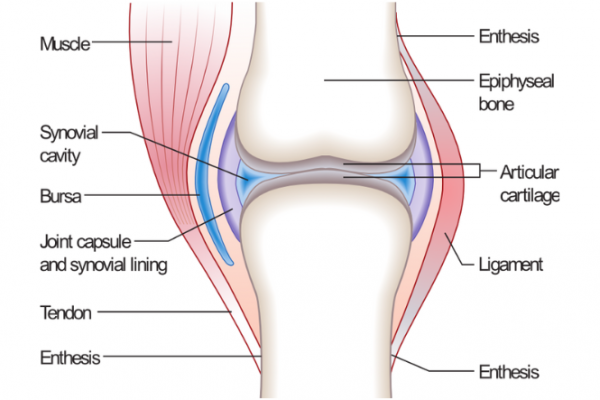
Image credit: Madhero88 via Wikimedia Commons(external link)
Video: What is juvenile idiopathic arthritis?
(Arthritis NZ, 2021)
JIA is more common in girls than boys and can occur at any age under 16. The exact causes are not known – current research indicates that genetic factors may play a part and infection or viruses may trigger the condition.
JIA usually affects the knees, hips, hands and feet, although other joints may be involved as well.
Symptoms include:
- joint pain, swelling, tenderness, stiffness, redness and warmth
- fatigue, fevers, loss of appetite or weight, and generally feeling unwell
- skin rashes
- swelling in lymph glands
- inflammation of the eyes (uveitis) and other organs of the body.
Most common types of JIA
- Oligoarthritis (from ‘oligo’ meaning few) occurs when up to 4 joints are affected, usually the knees and ankles. Children may also develop eye inflammation (iritis or uveitis).
- Polyarticular (from ‘poly’ meaning many). This type involves 5 or more joints, with the same joints on each side of the body affected, including fingers, toes, wrists, ankles, hips, knees, neck and jaw.
Other, less common, types of JIA
- Systemic onset JIA (also known as Still’s disease). This usually includes fevers and rashes, and may cause inflammation of the internal organs. Symptoms may be confused with other childhood diseases, eg, measles or glandular fever.
- Enthesitis-related arthritis (ERA) describes inflammation of the ligaments and tendons around the joints. It most commonly affects the spine, heel, hips, knees and ankles.
- Psoriatic arthritis can affect any number of joints and is usually associated with psoriasis, a scaly skin rash that may also affect the nails.
There is no single test for JIA and reaching a diagnosis may take time, which can be very frustrating for families. Your child will be referred to a paediatrician who will work with a paediatric rheumatologist (who specialises in children with arthritis).
Diagnosis will be based on medical history, physical examination, blood tests, X-rays and other tests. Some of these are to rule out other diseases that cause pain and swelling in the joints, and they may need to be repeated.
Every child’s JIA is different and treatment may seem like ‘trial and error’ to find what works best. Your child is still growing, so their condition needs to be monitored closely and changes to treatment will be made from time to time. The overall aim is for your child and whānau to lead as normal a life as possible.
Treatment will depend on:
- what form of JIA your child has
- which joints are affected,
- how active the condition is
- how your child responds to the medicines prescribed.
The good news is that if JIA is diagnosed early and managed well, most children will outgrow it. About half of children with JIA may not need treatment as adults.
Medicines
- Pain relievers (analgesics) can help your child feel more comfortable, be more active and sleep better but they don't reduce inflammation.
- Non-steroidal anti-inflammatory drugs (NSAIDS) reduce inflammation and control stiffness and swelling, but they don't cure JIA. The most common side effects are stomach upsets.
- Disease-modifying anti-rheumatic drugs (DMARDS), eg, methotrexate, can slow the progression of JIA by ‘calming’ the overactive immune system. They take several months to reach maximum effectiveness. Some children are more likely to catch infections and they should not be give live virus vaccinations (eg, measles, mumps, rubella, oral polio, chicken pox) while on DMARDS.
- Corticosteroids are hormones that are produced naturally by the adrenal glands. As medicine, they can rapidly reduce pain and inflammation. They are most commonly given by injection into the inflamed joints.
- Biological therapies (biologics) are used to control pain, swelling and stiffness when DMARDS are not effective to control. Etanercept, adalimumab and tocilizumab are funded for JIA in Aotearoa New Zealand. They suppress the immune system so your child may be more likely to catch infections and should not be given live vaccinations while taking biologics.
Arthritis NZ has useful information about your child’s healthcare team and medicines that might be involved(external link).
Exercise
Physical activity is essential for good health and wellbeing in children with JIA. Exercise helps reduce the pain of JIA, keeps muscles and bones strong, and improves confidence. You will need to find physical activities and sports that your child enjoys but that don’t cause too much discomfort. Your child’s physiotherapist can advise on suitable activities and exercises. Swimming is great as it allows freedom of movement and it’s fun!
JIA can cause tiredness so it’s important they get a good night’s sleep and maybe some rest during the day. Rest doesn’t mean lying in bed all day as this can lead to further stiffness and loss of mobility. Try activities like listening to music, reading, and artwork instead.
Healthy eating
Children with JIA can have trouble with their appetite, so it’s important to make sure they are eating enough to maintain a healthy weight and energy levels. A balanced diet is important, including plenty of fresh fruit and vegetables, and calcium-rich dairy products like milk, cheese and yoghurt. Read more about healthy eating for children(external link).
Managing pain and flares
Flares can happen after infections, periods of stress or changes in medicines but they can also happen for no apparent reason at all. During a flare, your child may be in greater pain, their joints may be swollen and stiff, and they may be tired yet have trouble sleeping. In turn, this may affect their mood – leading to an ongoing cycle of pain and distress.
Together with your child, you can learn some strategies that will help them through a flare, eg, deep breathing and relaxation techniques. You can also try hot and cold packs, massage, gentle stretching exercises and distraction.
Emotional and social support
JIA can be a challenge for you and your child as well as siblings and other family members. It may be difficult to explain what is happening during a flare. A team approach to managing your child’s arthritis will help, along with support from family, friends and teachers. Many families find it valuable to connect with others who are living with JIA, through the Arthritis New Zealand annual Children’s Camp.(external link)
The short video below gives an overview of the 2023 teens camp in Wellington.
Video: Abbvie video
Arthritis NZ has more information about:
- what you can do as a parent or caregiver for children with arthritis(external link)
- talking to teachers(external link)
- your health team(external link).
Apps reviewed by Healthify
You may find it useful to look at some Arthritis apps.
It can be a challenging time for living with JIA as teenagers and young adults deal with the challenges of transitioning from high school in to further education, training or work, as well as transitioning from paediatric to adult rheumatology services. In addition, there are the pressures of balancing the management of JIA, with keeping up a normal life with hobbies, sports, social and school activities. Arthritis Australia have a useful handbook(external link), however do keep in mind that some information will be specific to Australian services.
- Arthritis can vary from child to child. Your doctor will create a treatment plan(external link) specifically for your child.
- Be prepared for flares – know how to recognise and manage a flare.
- Encourage your child to participate in normal activities, eg, sports, crafts, music.
- Explain to friends and teachers at your child’s school(external link) what juvenile arthritis is and how it might affect your child’s daily life.
- Encourage regular school attendance and daily routines.
- Write down questions as you think of them, ready for the next time you talk with your child’s healthcare team.
- Encourage your child to learn their own limits, try new things, and manage aspects of arthritis themselves, eg, taking medicines.
- Don’t be afraid to reach out for help and support.
VIDEO: Juvenile Idiopathic Arthritis (in pre-schoolers)(external link) Arthritis NZ
Children with arthritis(external link) Arthritis NZ
Children’s camps(external link) Arthritis NZ
Children with arthritis – what can you do?(external link) Arthritis NZ
Children with arthritis – talking to teachers(external link) Arthritis NZ
Children with arthritis – your health team(external link) Arthritis NZ
Apps
Brochures
Juvenile Idiopathic Arthritis(external link) Arthritis NZ
Living with arthritis – A guide for young adults(external link) Arthritis Australia
Dealing with anxiety(external link) The Lowdown, NZ
References
- Children with arthritis(external link) Arthritis NZ
- JIA (Juvenile Idiopathic Arthritis)(external link) Arthritis NZ
Brochures

Living with arthritis – A guide for young adults
Arthritis Australia
Credits: Arthritis New Zealand. Edited by Healthify editorial team in 2024. Healthify is brought to you by Health Navigator Charitable Trust.
Page last updated:





