If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Abdominal hernia | Mate whaturama
Key points about abdominal hernia
- An abdominal hernia (mate whaturama) is when an internal part of the body, commonly a piece of bowel, pushes through a weak part of your abdominal (tummy) wall muscle and creates a bulge or lump.
- Usually, you can push the hernia back in or it disappears when you lie down, but assessment and treatments may be recommended so it doesn’t get larger or become painful.
- Hernias can become stuck or strangulated, where the tissue poking out gets trapped by the muscle.
- If your hernia is firm or tender and can’t be pushed back in, or you have sudden severe pain, vomiting or difficulty passing stools (constipation) or wind, seek immediate medical help.

The word hernia means ‘something coming through’. The most common place for a hernia is the abdominal wall – a large sheet of muscle and tendon that helps hold all the abdominal content in place.
If there is an area of weakness in the wall, pressure from inside the wall can cause part of the abdominal contents (eg, the intestines) to be pushed through the opening. This resulting bulge is known as a hernia.
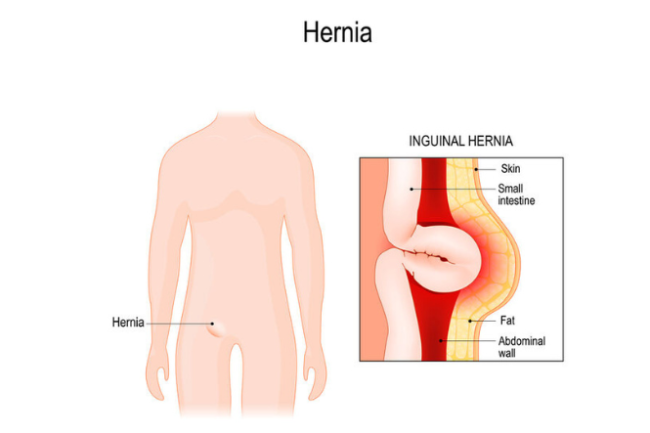
Image credit: 123rf
There are several common types of hernia:
- Inguinal hernias occur near your groin and are more common in men.
- Femoral hernias occur where your leg joins your body and are more common in women.
- Incisional hernias occur where you have a scar from surgery.
- Umbilical hernias occur near your naval (belly button) and are more common in newborns or people who are obese.
- Hiatus hernias occur when part of your stomach pushes up into the chest.
Hernias can affect anyone and many babies are born with hernias.
Abdominal hernias are caused by straining that puts pressure on that abdominal (tummy) area. Pressure may come from:
- constant coughing or sneezing
- being overweight
- lifting, carrying or pushing heavy loads
- constipation, leading to straining on the toilet
- pregnancy.
Some people have weaker abdominal walls which makes them more prone to hernias.
You may have no symptoms, or you may feel the following:
- a lump or bulge in your abdomen (tummy) or groin
- a heavy or uncomfortable feeling in your gut, particularly when bending over
- pain or aching after exertion, eg, after lifting or carrying heavy objects
- digestive upsets, eg, constipation.
Your healthcare provider will be able to make a diagnosis based on your symptoms and a physical examination. If the belly button (umbilicus) becomes red, hot, tender or your baby becomes unwell, irritable or is not passing bowel motions (poo), seek urgent medical help. 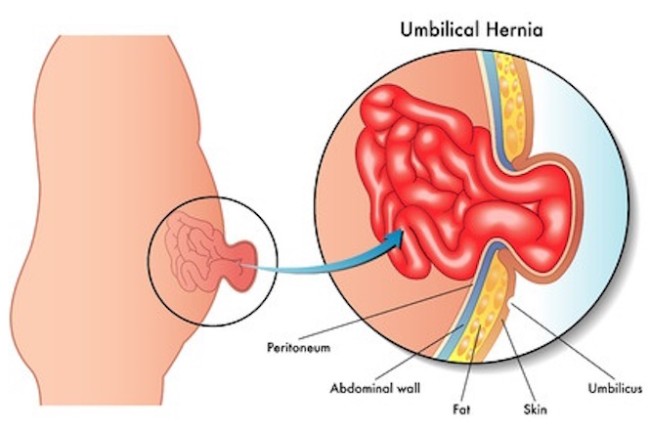
Image credit: 123rf
Many hernias don’t need treatment. Your healthcare provider will advise you to avoid heavy lifting and help you manage any conditions which contribute to symptoms, such as chronic cough or constipation.
If your hernia pops out and doesn’t go back by itself, you can get it in again by lying down and pushing it back with slow constant pressure. This can take a few minutes. If it doesn’t go back in, you can try putting an ice pack on it for a few minutes before trying again. If you can’t get it back in, see your healthcare provider.
If this happens and your hernia is extremely painful you need to go to hospital straight away because it may be strangulated. This is when part of your bowel or it’s supporting tissues get stuck in the weak part of your muscle wall and the blood supply to it is cut off.
Some types of hernia are more likely to strangulate. To prevent this from happening, these types of hernia are treated with surgery. It’s more likely you’ll have your hernia operated on if it:
- is affecting your day-to-day quality of life
- is an incisional hernia which is small or part of a stoma
- is a femoral hernia
- is very large
- has been hard to reduce (put back in place) on another occasion.
Surgery
If you do need surgery, it may be done under local or general anaesthetic. An incision (cut) will be made in your abdomen (tummy/puku) around the hernia, and the protruding piece of tissue (usually bowel) will be put back where it should be. Stitches or surgical mesh will be used to close the weak section of muscle or provide reinforcement.
- Inguinal hernias (near your groin) may be done with open or laparoscopic (keyhole) surgery. To make the repair stronger than just using stitches, surgical mesh is usually used. It’s stitched or glued over the opening and eventually it becomes part of the muscle layer.
- Femoral hernias (where your leg joins your body) are generally done early as there is an increased risk of strangulation. Mesh is usually used.
- Incisional hernias (from a surgery scar) can vary a lot in size. Mesh is usually used, especially for large ones.
- Umbilical hernias (near your belly button) are often repaired just with stitches, but larger ones may require mesh.
If surgery is too risky for you because of other health conditions, your healthcare provider may arrange a truss, corset or binder to help with symptoms instead.
Most people recover without any complications. If surgical mesh has been used in your hernia repair it can, rarely, cause problems or infections.
You can expect the wound area to be bruised and you may get some swelling. Bruising often moves downwards from the wound and, if you have them, into your scrotum and penis. It can look alarming but usually settles within a week or two.
You can expect to have some pain for up to 1 week. Panadol or ibuprofen (if you can take it) should be enough, if you need stronger pain relief talk to your healthcare provider.
You may have stitches or steristrips holding your wound together. You’ll be told what to do to look after your wound (eg, when to remove the dressing) and whether you need to have any stitches removed. Have a shower rather than a bath for the first 10 days so that you don’t soak your wound, and pat the area dry.
Time off work will be needed for you to recover:
- If you’ve had a keyhole repair (laporoscopic) – 1 week if you have a sedentary job (sitting) and 2 weeks or more if you do physical work. You can return to driving once you feel able to drive safely – when you can think clearly, your reaction time is back to normal and you can press the pedals without discomfort.
- If you’ve had open surgery or a larger repair you’ll need about 4 weeks off work and may need to be checked by your surgeon before you go back to work or return to driving.
It’s important to stay active to keep your blood circulating and reduce the risk of deep vein thrombosis (DVT). If you feel tired, sit and put your feet up for a while but it’s best not to go to bed during the day.
When to get help
Go back to your healthcare provider if:
- you develop a fluid-filled lump (seroma)
- there is bleeding at the wound site
- there are signs of infection (redness, swelling, pus) at the surgical site
- you have a fever or flu like symptoms
- you have severe groin or testicle pain
- you have pain in your calf (lower leg) or feel breathless.
Seeing your healthcare provider is the best way of helping yourself if you have a hernia. Some devices (eg, hernia trusses, support belts) and therapies are available (eg, physiotherapy and medication for cough and constipation) to reduce symptoms and ease discomfort. Talk to your healthcare provider about whether they are suitable for you.
You can reduce your chances of getting a hernia if you:
- eat lots of high fibre foods to stop you getting constipated
- maintain a healthy weight
- take care when lifting heavy object by bending from your knees, not your waist
- get treatment if you have a persistent cough or sneeze
- quit smoking as this can cause persistent coughing, which can put pressure on your abdominal wall.
Apps reviewed by Healthify
You may find it useful to look at some Nutrition, exercise and weight management apps and Quit smoking apps.
Talk to your healthcare provider and, if you need additional support, they can help you to access other healthcare professionals such as physiotherapists and counsellors.
Hernia(external link) Patient Info, UK
Hernia(external link) Better Health, Australia
Umbilical hernia in kids – pre-referral guidelines(external link) Royal Children's Hospital, Australia
Hernia(external link) What is a hernia video, NHS, UK
Apps
Nutrition, exercise and weight management apps
Quit smoking apps
References
- LeBlanc KE, LeBlanc LL, LeBlanc KA. Inguinal hernias – diagnosis and management(external link) Am Fam Physician 2013;87(12):844-48
- Brooks DC, Hawn, M. Classification, clinical features and diagnosis of inguinal and femoral hernias in adults(external link) UpToDate, US, 2022
- Inguinal hernias(external link) Patient Info, UK, 2022
- Hernia(external link) Patient Info, UK, 2023
- Hernia in adults(external link) Auckland Regional HealthPathways, NZ, 2023
- Groin hernia and you(external link) British Hernia Society, UK
- Hernia repair surgery(external link) Health New Zealand | Te Whatu Ora, NZ
Clinical diagnosis and treatment
- Identify the source of the hernia and describe pertinent features, eg:
- inguinal, umbilical, abdominal, femoral
- traumatic, post-operative or spontaneous
- direct versus indirect inguinal hernia
- reducible versus non reduceable
- history of ‘red flag’ symptoms such as severe pain, constipation and vomiting.
- Consider urgent medical assessment of hernia with red flag symptoms or signs of shock, peritonitis etc.
- Ultrasound is not required for diagnosis of hernia and is unlikely to change the surgical management (see HealthPathways(external link)). Use POCUS or refer for ultrasound if source of lump is unclear.
- Post-operative (incisional) hernia may be covered by ACC (see ACC Abdominal Wall Hernia as Treatment Injury; Guide to Cover(external link)).
- Hernias may be the underlying cause of other conditions such as severe GORD, see Gord BPAC 2014(external link) or urinary incontinence, see Urinary incontinence BPAC 2014(external link)
- Hernia may be exacerbated by other health conditions such as high body weight, separation of the abdominal muscles, chronic cough or respiratory disease, chronic constipation, urinary obstruction, pregnancy and postpartum.
- Differential diagnoses may include hydrocele, lipoma, femoral lymphadenopathy and more.
| Property | Inguinal hernia | Femoral hernia |
| Sex | More common in male patients | More common in female patients |
| Defect | Pass through inguinal canal | Pass through femoral canal |
| Site | Above and medial to pubic tubercle Above the crease of the groin |
Below and lateral to pubic tubercle Below the crease of the groin |
| Strangulation | Less common | More common because of rigid neck – Ricter's hernia |
| Treatment | Can be treated without surgery | Surgery is essential because of risk of strangulation |
| Reduction | Can be reduced completely | Cannot be reduced completely |
| Cough impulse | Cough impulse usually present | Many do not have cough impulse |
Source: Table from Southern Health Pathways – Hernia in adults (2022)
There are 2 issues to consider regarding treatment:
- Watchful waiting versus early elective surgical repair. See management policy for asymptomatic inguinal hernias(external link) NSMJ, 2015
- The use of mesh versus sutures in surgery. See long-term recurrence and complications associated with elective incisional hernia repair(external link) JAMA, 2014
Summary
- Refer when concern for red flag symptoms and include these in your assessment.
- Inguinal hernia are common and one third are asymptomatic or minimally symptomatic.
- Most centres will prioritise referrals where the hernia is large and the patient is significantly symptomatic (Bagshaw, NZMJ 2015).
- Before referring for surgery, give patient advice on what to expect after surgery.
Resources
For useful information on post-operative care after hernia surgery, see Post-operative care(external link) British Hernia Society.
What to expect after surgery
- Most patients recover without complications. Mesh rarely causes complications in hernia repair, and 1 in 3,000 patients get local mesh infection. See New Zealand Association of General Surgeons Position Statement: Mesh Hernia Repair(external link).
- It is normal for the scrotum and groin to be black and bruised.
- You can return to driving once you feel able to press pedals.
- Expect some pain for up to 1 week.
- To enhance recovery, 1–2 weeks of time off will be required (1 week if sedentary work, 2 weeks if physical labour).
- Return to your general practice if you develop a lump.
Source: Southern Health Pathways – Hernia in Adults (2022)
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Bryony Harrison
Last reviewed:
Page last updated:





