Haemorrhoids | Mate tero puta
Also known as piles
Key points about haemorrhoids (mate tero puta)
- Haemorrhoids are clusters of veins that sit just under the surface tissue of your rectum (the last part of your bowel) and your anus (the opening of your bowel).
- The condition we think of a haemorrhoids (mate tero puta), or piles, is when these veins become swollen with blood, like varicose veins.
- They can form internally in your rectum and externally around your anus (bottom).
- Haemorrhoids can be painful, itchy and can bleed – especially when you have a bowel motion (poo).
- They're common and can often be managed with self-care and by changing your diet and bowel habits.
- If self-care doesn't work, there are treatment options available.

Internal haemorrhoids
When haemorrhoids occur inside your rectum they’re known as internal haemorrhoids. You may not know you’ve got them, but symptoms can include:
- Seeing small smears of bright red blood (on the toilet paper when you wipe or in the toilet) after you poo.
- Feeling like you still need to poo after you’ve been.
- Seeing mucus in your underwear or on the toilet paper after wiping your bottom.
They’re not usually painful, even when they bleed, but sometimes a haemorrhoid can drop down through your anus (prolapse). They look like reddened, puffy lumps, and can become painful and get irritated and itchy.
External haemorrhoids
Haemorrhoids you can see or feel around your anus are called external haemorrhoids. They look or feel like firm, grape-like swellings on the outside of your anus.
These are usually more painful as they are more exposed. They can itch and bleed. Sometimes a blood clot (called a thrombus) can form in a haemorrhoid. This can be very painful, and can create a hard, discoloured lump near your anus.
Sometimes when a swollen haemorrhoid settles down, the skin that was stretched over it stays loose. This is called a skin tag and although it shouldn't hurt it can make cleaning your bottom after a bowel motion more difficult. You could try using a moist cloth or non-scented wet wipe.
Haemorrhoids are common – about 50% of adults (1 in 2) have them after 50 years of age.
The image below shows the location of internal and external haemorrhoids. Note that the US spelling is 'hemorrhoids'.
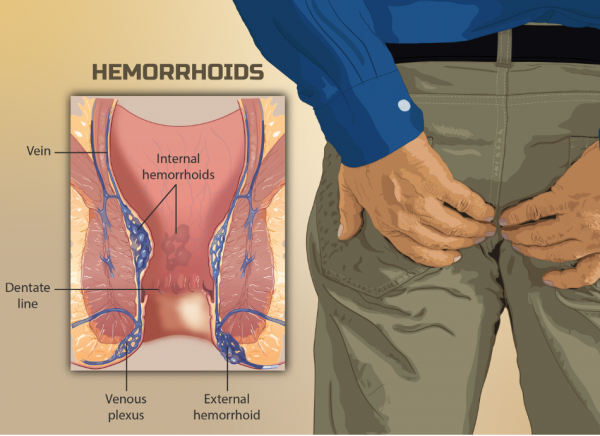
Image credit: myupchar.com(external link) via Wikimedia Commons
Make an appointment
See your healthcare provider if you have:
- symptoms of haemorrhoids and they’re not improving (or they’re getting worse) following self-care at home (see below)
- haemorrhoids that keep coming back
- a change around your anus that doesn’t seem normal.
Get help urgently
Get medical help urgently if you have symptoms and:
- you also have a high temperature or feel unwell
- you have an infected haemorrhoid (there’s yellow discharge leaking from it).
Your healthcare provider will ask you questions about your symptoms. They may need to examine your rectal area (where you poo) to look for signs of piles and any complications. If there’s evidence of blood in your poo, you may need more tests (eg, a colonoscopy) to make sure there’s no other cause.
Haemorrhoids can develop when there’s an increase in pressure on the veins around your rectum and anus.
The increased pressure may be caused by:
- prolonged straining or pushing to pass a bowel motion (poo), which can happen when you are constipated(external link)
- diarrhoea(external link)
- being overweight (having a high BMI)
- having a diet that’s low in fibre
- sitting on the toilet for a long time
- getting older – the connective tissue around your haemorrhoids can get weaker allowing them to prolapse
- heavy lifting or coughing
- pregnancy and childbirth
- having anal intercourse
- a family tendency for haemorrhoids.
Haemorrhoids can get better by themselves after a few days, but larger haemorrhoids may take longer to heal and you may need medical advice or treatment.
Here are some things you can do to manage haemorrhoids, and avoid getting them again.
When you have haemorrhoids
- Apply a cold compress to the area for relief.
- Sit in a warm bath which can help the pain and itching. Pat yourself dry afterwards.
- Treat any constipation and avoid food and drinks that can make it worse, softer stools are easier to pass.
- Clean yourself carefully after a bowel motion. Don’t rub or wipe too hard.
To prevent haemorrhoids
- Eat a high-fibre diet (eg, plenty of fruit, vegetables, wholegrain bread).
- Drink plenty of fluids (ideally water) and avoid too much alcohol and sugary drinks.
- Exercise regularly.
- Sit on a cushion rather than a hard surface.
- Always go to the toilet as soon as you feel the need to go. 'Holding-on' can make haemorrhoids worse.
- Use a good toileting position:
- Your knees higher than your hips, feet flat on floor, lean forwards and put your elbows on your knees, bulge out your abdomen (tummy, puku), and straighten your spine.
- Using a small footstool to raise and support the feet can assist in getting your knees higher than your hips.
- Avoid straining or staying on the toilet for longer than you need to.

Image credit: Healthify He Puna Waiora
Apps reviewed by Healthify
You may find it useful to look at some Nutrition, exercise and weight management apps.
Topical treatments (creams) and suppositories.
There are prescription and over-the-counter topical products, including suppositories, that may help reduce mild discomfort, swelling and itching. Using these products after they’ve been stored in the fridge can provide an additional cooling effect.
Talk to your healthcare provider or pharmacist first to be sure these are safe for you, and to make sure there isn't any other underlying medical condition that needs different treatment. Also ask about how long to use the topical treatments and when to seek extra help if they’re not working.
Procedures
If self-care and topical treatment doesn’t work, there are several procedures your healthcare provider can discuss with you.
Non-surgical procedures include:
- Banding – when a band is placed around the base of the haemorrhoid to remove the blood supply and cause it to shrink
- Electrotherapy – a heat treatment causing the haemorrhoid to harden and shrivel
- Sclerotherapy – an injection into the haemorrhoid to make it shrink.
Surgical procedures
- A haemorrhoidectomy can be done to remove the haemorrhoid altogether.
- Haemorrhoid stapling also removes the haemorrhoid with a ring of staples around the base being used to prevent bleeding.
Piles – an overview(external link) NHS Choices, UK
Haemorrhoids(external link) Patient Info, UK
Apps
Nutrition, exercise and weight management apps
References
- Hemorrhoids(external link) Mayo Clinic, US
- Hemorrhoids and what to do about them(external link) Harvard Health Publishing, US, 2021
- Local preparations for anal and rectal disorders(external link) New Zealand Formulary, NZ, 2023
- Haemorrhoids(external link) 3D pathways, NZ, 2022
- Piles (haemorrhoids)(external link) NHS, UK, 2022
- Choice of treatment for haemorrhoids is highly dependent on symptoms(external link) NZ Doctor, NZ, 2021
- Toilet positions(external link) Bladder & Bowel Community, UK
A quick guide to managing anal fissures(external link) Best Practice Journal, NZ, 2013
Topical creams and preparations(external link) NZ Formulary
Hydrocortisone + cinchocaine (Proctosedyl)(external link) NZ Formulary
Cinchocaine + fluocortolone hexanoate + fluocortolone pivalate (Ultraproct)(external link) NZ Formulary
Haemorrhoids - a review(external link) RACGP Australia
Apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Last reviewed:





