Guillain-Barré syndrome
Sounds like 'gee-YAN bah-RAY'
Key points about Guillain-Barré syndrome
- Guillain-Barré syndrome (GBS) is a rare autoimmune disorder affecting nerves. Autoimmune means that the body attacks itself, without any real known cause or reason.
- The cause is unknown, but GBS often occurs after a viral or bacterial infection.
- It's more common in older people and more men than women are affected.
- It causes muscle weakness, loss of reflexes and numbness or tingling (pins and needles) in the arms, legs, face and other parts of the body. In severe cases it can cause complete paralysis.
- It stops getting worse within 4 weeks and most people get better over the next 12 months.

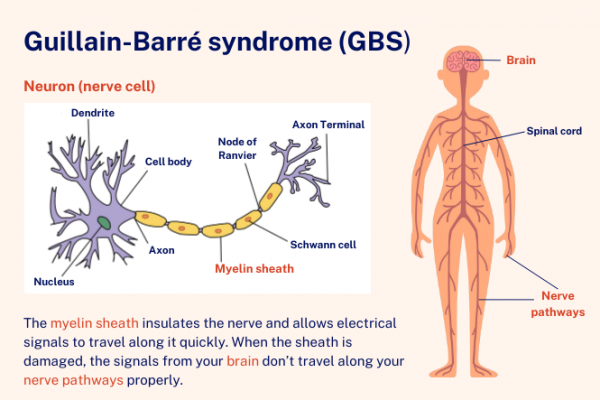
Image credit: Healthify
Guillain-Barré syndrome happens when your immune system attacks and damages your peripheral nerves. Your peripheral nerves are the nerves in your body, arms and legs – the ones outside your brain and spinal cord. Guillain-Barré syndrome (GBS) is a group of similar diseases affecting different parts of different nerves. The commonest ones are:
- Acute inflammatory demyelinating polyradiculoneuropathy (AIDP): This is the most common form. Your immune system attacks the myelin sheath, which is a fatty layer around the nerve that makes the electrical signal travel faster.
- Acute motor axonal neuropathy (AMAN) and acute motor-sensory axonal neuropathy (AMSAN): Your immune system attacks the nerve itself, called the axon.
Video: Guillain-Barré syndrome (GBS) 101
The video below gives an overview of GBS, how it affects you, its treatment and recovery. It may take a few moments to load.
(GBS-CIDP Foundation International, US, 2015)
The exact cause of Guillain-Barre syndrome is unknown, but most people who develop it have had some sort of infection in the few weeks before getting symptoms. The infection may have been:
- food poisoning (especially Campylobacter which is common in Aotearoa New Zealand)
- flu
- a viral infection, eg, HIV, EBV (glandular fever), Cytomegalovirus (CMV), COVID-19
Less commonly, GBS may follow:
- some tropical diseases, eg dengue and the Zika virus
- surgery or trauma
- bone marrow transplant
- immediately after childbirth (very rare)
- vaccination (very rare – getting the flu is a greater risk).
GBS is not hereditary (you don’t inherit it from your parents) and it’s not infectious or contagious (you can’t catch it or pass it on to anybody else).
GBS usually:
- starts with weakness and tingling in the feet
- moves up your body
- develops over a few days to 2 weeks
- is at it’s worst after 4 weeks
- has symptoms that are symmetrical, that is they are equal on both sides of your body.
GBS can be mild or more severe, and has different symptoms for different people. Symptoms can include:
- difficulty with walking – your legs may feel heavy, wooden and weak
- balance and coordination problems
- weakness and tingling in your arms
- weakness of the diaphragm, which causes difficulty breathing
- numbness
- pain
- weakness, numbness or tingling of your face including around your mouth and lips
- blurred vision
- problems with chewing, swallowing and speaking
- problems with peeing and constipation (hard to pass poo)
- fever
- heart rate going fast or slow
- blood pressure going up and down causing dizziness.
If you think you could have GBS make an urgent appointment to see your GP or nurse practitioner. They will ask when your symptoms started and how they have changed, and whether you've had any recent infections. They’ll examine you to test for weakness. If they think you may have GBS they’ll send you to hospital for further assessment. At the hospital other tests could include:
- a blood test
- a spirometry test to see how well you’re breathing
- an ECG
- a lumbar puncture to take a sample of cerebrospinal fluid – this is the test which gives the most information about whether you’re likely to have GBS or something different
- a nerve conduction study.
There’s no cure Guillain-Barré syndrome, but it usually gets better on its own as the nerves repair themselves. Most people with GBS will be admitted to hospital, where your breathing, heart rate, and blood pressure can be carefully tracked. You will probably be given to following:
- Special supportive stockings and medicine to try and prevent you from getting blood clots in your legs (DVT) because you’re not moving around as usual.
- Pain relief with medicines that work well for nerve pain.
- Physiotherapy and occupational therapy to help to build up strength and flexibility.
- If your GBS is severe, you may be treated with:
- Plasma exchange where blood is taken out of your body, the harmful antibodies are removed from the blood, and then the blood is returned to your body.
- Intravenous immune globulins – helpful antibodies that are added to your blood.
Hospitals need special facilities to care for people with GBS, so if you’re in a rural part of Aotearoa New Zealand, you may need to be admitted to a hospital in a major town at first. You may need to be cared for in an intensive care unit (ICU) and need a ventilator to help you breathe until your nerves recover.
GBS symptoms usually get to their most severe (strongest) within 4 weeks. They can then stay the same for weeks or months before gradually getting better. Some people have a relapse after starting to improve (about 1 in 10). Most people with Guillain-Barré syndrome will make a full recovery within 12 months. However, you may be in hospital for a few months. Depending on how severe your GBS was and what type you had, you may need many months of physiotherapy and occupational therapy. About 2 or 3 in 10 people are left with ongoing difficulty walking. Other people continue to have tiredness, weakness, or pain.
Having GBS can be scary for you and for your whānau – especially if you have problems breathing. You may feel anxious or depressed and may have problems sleeping. You may also feel really tired. It’s important that you have support from family and friends as well as from your healthcare team. If you’re feeling distressed, ask for help.
There’s a national support group(external link) including people who have experienced Guillain-Barré syndrome themselves. They also have a private Guillain-Barré support group Facebook page(external link).
The following links provide further information on Guillain-Barre syndrome. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Guillain Barré Syndrome(external link) Guillain Barré Syndrome Support Group NZ Trust
Guillain-Barré Syndrome(external link) Patient Info, UK
References
Guillain-Barré syndrome(external link) NHS, UK, 2023
Guillain-Barré Syndrome(external link) Patient Info, UK
Guillain-Barre syndrome(external link) Mayo Clinic, US, 2022
Guillain-Barré syndrome in adults – pathogenesis, clinical features and diagnosis(external link) UpToDate, US, 2023
Guillain-Barré syndrome in adults – treatment and prognosis(external link) UpToDate, US, 2023
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





