Gingivitis (gum inflammation)
Key points about gingivitis
- Gingivitis is a common mild inflammation (redness and swelling) of your gums. It can be a sign of poor oral hygiene.
- It's usually caused by the build-up of plaque on your teeth due to not brushing and flossing regularly enough.
- Symptoms include red and tender gums, and bleeding when brushing or flossing.
- You can usually treat gingivitis at home yourself through good oral hygiene, such as gently brushing your teeth twice a day and flossing them once each day.
- If left untreated, gingivitis may progress into more serious gum diseases, known as periodontitis.

Gingivitis is a common and mild form of gum disease causing redness and swelling of the gums around the base of your teeth.

Image credit: Depositphotos
Gingivitis mostly occurs if you don’t look after your teeth properly, or if an area is often missed by your toothbrush by mistake, when cleaning your teeth. If your teeth aren’t cleaned well at home and checked regularly by a dentist, plaque can build up where your gums meet your teeth. If it’s not managed, gingivitis can lead to periodontal disease.
Gingivitis is a sign that there is excess bacteria and plaque in your mouth, which your body is fighting back against through inflammation. As your gums get inflamed, they can become puffy and bleed when you brush.
This happens because your mouth is full of all sorts of bacteria – some good for us, some bad. The bad bacteria, along with mucus and other particles, can form a sticky ‘plaque’ on your teeth. If you don’t brush and floss regularly, the plaque may harden from the calcium in your saliva and form ‘tartar’ (also known as ‘calculus’). Calculus increases the rate at which plaque forms, as it provides a base for the bacteria to live on. This causes inflammation of your gums, or gingivitis. It can't be removed at home, it needs a dentist or dental hygienist to carefully scrape it off – called scaling
It can be easy to overlook mild gingivitis. You may be unaware of it until your dentist or hygienist checks for it. Look out for the following symptoms:
- swollen red gums
- bleeding when brushing, flossing or eating
- tenderness or pain
- bad breath (halitosis)
- sensitivity to cold or hot foods and drinks.
Gingivitis can affect anybody but you're at increased risk if you:
- have poor brushing habits, which leads to plaque and tartar building up
- smoke
- have diabetes (especially if it's poorly controlled)
- are obese
- have a weakened immune system
- have a dry mouth (saliva is protective) – this can be caused by some medications and by getting older
- have poorly fitting dentures
- brush your teeth too hard
- are pregnant
- have a diet lacking in vitamins and minerals.
In most cases, you can treat gingivitis at home by following good oral hygiene practices. These include:
- gently brushing your teeth twice a day (first thing in the morning and before bed) with a fluoride toothpaste
- using a soft or ultra-soft toothbrush – medium and hard toothbrushes can damage your gums and can be less effective at removing plaque
- flossing regularly to remove plaque from between your teeth – if you have larger gaps between your teeth a dental professional might recommend you use an interdental brush
- considering using an electric toothbrush rather than a manual one
- using mouthwash daily after brushing to further reduce bacteria in your mouth.
For acute gingivitis, use a mouth rinse such as Colgate Savacol for up to 2 weeks (longer-term use may stain your teeth and it's the wrong type of mouthwash for long-term use). If your gingivitis is ongoing, use any supermarket type of mouthwash daily. If your gingivitis persists, see a dentist.
You should also:
- visit your dentist routinely for a check-up and professional cleaning
- avoid smoking and limit alcohol intake
- avoid cannabis use as this is associated with severe gingivitis and periodontitis
- avoid eating sugary foods between meals.
If it's not treated, gingivitis may develop into more deep-seated inflammation and infections in your mouth, such as periodontitis (periodontal or gum disease), although this doesn’t always happen. Periodontal or gum disease can destroy the ligaments and bone holding your teeth securely in place so that they become loose and teeth may eventually fall out.
Gingivitis can also lead to acute necrotising ulcerative gingivitis, which is a condition that causes pain, tissue loss and foul breath.
Prevention is the same as treatment. If you follow the steps outlined under treatment, you have much less risk of developing gingivitis.
Avoiding smoking is a key step in keeping your gums healthy. People who smoke have a higher risk of gum problems (and oral cancer), such as complications after tooth extractions and surgery in your mouth. You have lower resistance to infections and your healing is impaired.
Gum conditions in smokers are also often not noticed. This is because people who smoke typically don't have bleeding gums as they have poor blood supply to their gums. If you're a smoker and you stop smoking, your gums are likely to start to bleed. This is because the blood supply is returning to your gums and they're starting to fight the plaque.
Apps reviewed by Healthify
You may find it useful to look at some Quit smoking apps.
The following links provide further information about gingivitis. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Oral hygiene(external link) Patient Info, UK
Gum disease(external link) NHS Choices, UK
Gingivitis and periodontal disease(external link) WebMD
Apps
Resources
It's easy to protect your family's smile(external link) HealthEd, NZ Available in the following languages: English(external link), Cook Islands Māori(external link), te reo Māori(external link), Niuean(external link), Samoan(external link), Tokelauan(external link), Tongan(external link)
Take care of your teeth(external link) HealthEd, NZ
Periodontal disease(external link) HealthEd, NZ
References
- Gingivitis(external link) Mayo Clinic, US, 2023
- Chapple IEC et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium(external link) J Clin Periodontol. 2018 Jun;45 Suppl 20:S68S77
- EL Morelli, JM Broadbent, JW Leichter, WM Thomson. Pregnancy, parity and periodontal disease(external link) Australian Dental Journal 2018;63:270–278
- Robinson P, Deacon SA, Deery C et al. Manual versus powered toothbrushing for oral health(external link) Cochrane Database Syst Rev 2005; CD002281.
- Effects of smoking and vaping on oral health(external link) Better Health Australia, 2021
See also pages for clinicians on gum conditions and periodontitis
EL Morelli, JM Broadbent, JW Leichter, WM Thomson. Pregnancy, parity and periodontal disease(external link) Australian Dental Journal. 2018;63:270–278
Robinson P, Deacon S A, Deery C et al. Manual versus powered toothbrushing for oral health(external link) Cochrane Database Syst Rev 2005; CD002281
Some dental and periodontal diseases(external link) Patient Info Professional, UK, 2014
Chapple IEC, Mealey BL, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium.(external link) J Clin Periodontol. 2018 Jun;45 Suppl 20:S68-S77
Papapanou PN, Sanz M, et al. Periodontitis – consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri‐implant diseases and conditions(external link) Clin Periodontol. 2018;45(Suppl 20):S162–S170.
Brochures
HealthEd, NZ, 2022
English, Cook Islands Māori, te reo Māori, Niuean, Samoan, Tokelauan, Tongan
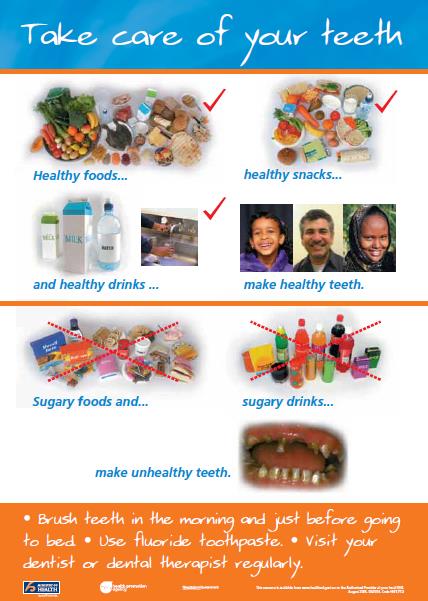
HealthEd, NZ, 2020
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Sophie McKenna, General Dental Surgeon
Last reviewed:





