You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
COVID-19 positive: Caring for your child at home
How to care for your child if they get COVID-19
Key points about caring for your COVID-19 positive child at home
- If your child is COVID-19 positive, this guide (developed with KidsHealth NZ) will help you care for your child at home and know when to ask for help.
- Most children with COVID-19 get mild symptoms or none at all.
- A small number will become more unwell and need extra care from their doctor, or in hospital.
- Children with COVID-19 can still get other illnesses. If you are worried about your child you can still get help for them even though you are keeping close to home.
- Know what to look out for, keep track of your child's symptoms and know when to ask for help and how to get it.
Most children with COVID-19 get mild symptoms or none at all. A small number will become more unwell and need extra care from their doctor, or in hospital. Children with COVID-19 can still get other illnesses.
Use these three steps:
- Recognise – know what to look out for to tell if your child is becoming unwell. See What to expect in the next accordion.
- Record – keep track of your child’s symptoms using a diary. Some children will also get a pulse oximeter. This is for checking oxygen levels.
- Respond – know when to ask for help and how to get it. See the advice below about how to manage symptoms at home, and what to do if your child becomes unwell.
Most children will have mild COVID-19 symptoms for up to 2 weeks. Symptoms tend to appear around 2-5 days after a person is infected but can take up to 14 days to show.
Days 1–3
Early symptoms of COVID-19 vary widely.
- Sometimes it begins with a sore/upset tummy or a bout of diarrhoea (runny poo) or vomiting (being sick).
- It can start with a tickle in your throat, a cough, fever or headache. Your child may also have difficulty breathing. Learn about the signs that a child is struggling to breathe.
- Some children feel tired and may lose their sense of taste and smell.
- Your child may have some or none of the above.
Days 4–6
These are important days to be more aware of your child's symptoms. This is when breathing may start to get worse.
- Your child may start to feel worse and may have aches, chills, a cough and be unsettled or irritable.
- Some children may develop rashes, including itchy red patches, swelling or blistering on the toes or fingers.
Days 7–8
- For children with mild illness, the worst is generally over after a week.
- Some children may get worse at this point, or start to feel better briefly then take a turn for the worse.
- There is more detail about how to tell if your child needs more help, and how to get it, in the section below on recognising and responding if your child becomes unwell.
Days 8–12 (week 2)
- Continue to monitor your child's symptoms and record them in your diary.
- There is more detail about how to tell if your child needs more help, and how to get it, in the section below on recognising and responding if your child becomes unwell.
Days 13–14
- Most children will feel better by now. Some may feel more tired than usual.
- It is best for your child to return to activity slowly.
- If your child has ongoing symptoms, your healthcare team will let you know what to do.
From 2–6 weeks
A very small number of children develop a serious condition after having COVID called PIMS-TS (Paediatric Inflammatory Multisystem Syndrome Temporally associated with SARS-CoV-2). Children with this condition can have the following problems:
- fever lasting for 5 or more days
- breathing difficulty
- tummy pain, vomiting or runny poo (diarrhoea)
- red lips or tongue
- red eyes
- a skin rash
- cold or swollen hands or feet.
There is more detail about how to tell if your child needs more help, and how to get it, in the section below on recognising and responding if your child becomes unwell.
Keeping track of your child’s symptoms and how they are feeling helps you and the healthcare team looking after them know if your child becomes more unwell. Make a record of the following things 3 times a day in your diary:
- cough
- breathing effort
- vomiting
- diarrhoea
- temperature (see: instructions for using a thermometer(external link))
- breathing rate
- how they are overall.
If you have been given a pulse oximeter for your child also record the following things.
- pulse rate
- oxygen level.
It is important you get an accurate measurement so check the instruction on how to use a pulse oximeter.
If you are worried about your child, ask for help. You could:
- call your healthcare team using the number given to you
- call the after-hours healthcare team using the number given to you
- call Healthline on 0800 611 116 if you are unsure about what to do
- dial 111 for urgent medical help.
Stay calm and explain why you are worried about your child, and tell them that your child is being looked after at home with COVID-19.
If you are waiting to hear back from your doctor and think that your child is getting sicker, call back and calmly explain why you are worried.
If you have already seen or talked to a doctor but your child is getting worse, call your doctor back and tell them what is happening.
|
Dial 111 and ask for urgent medical help if your child: |
|
Tell the operator your child has COVID-19. This will help them take the right precautions when they are looking after your child.
|
Call your healthcare team urgently if your child: |
|
Your healthcare team will plan with you when and how to check your child. This may involve seeing them on video or in person.
|
Call your healthcare team if your child has any of the following: |
|
Your healthcare team will plan with you when and how to check your child. This may involve seeing them on video or in person.
|
You can look after your child with a fever at home if they: |
|
Young babies (less than 3 months old) need a more cautious approach. If your child is under 3 months old and you are worried about them, call your healthcare team. Trust your instinct.
- If they have a fever, always call your healthcare team, who will figure out with you when and how to check them.
- If you are worried about them, call your healthcare team even if they do not have a fever.
- Some babies may have an unstable temperature with an infection - they may be colder than normal - in a sick infant this is a worrying sign and is a reason to call your healthcare team urgently.
- Babies get fevers for the same reasons as older children, but they are not as good at fighting off infections.
- When you call your healthcare team they will figure out with you when and how to check your baby.
Here is a video(external link) made by Starship Child Health on how to care for your child with COVID-19 at home.
There is no treatment that cures COVID-19, but there are things you can do to help your child with the symptoms it causes. The most important of these is you giving comfort, being reassuring, and distracting your child with books or playing with them.
Fever
- Undress your child so that they are just wearing a single layer (maybe a singlet and pants).
- Make sure the room is not too hot or too cold. These are the best and most comfortable ways to bring your child's temperature down.
- It's best not to give your child a bath or shower to cool them. You could use a cool face cloth.
- Your child may need extra rest or they may want to play – this is OK.
- Encourage them to drink fluids and eat healthy small meals.
Medicines
If your child is happy, and they are not unwell, you do not need to do anything more. You do not need to treat the fever with a medicine.
Paracetamol
If your child is miserable because of the fever, you can give paracetamol to make them more comfortable. You must follow the dosage instructions on the bottle. It is dangerous to give more than the recommended dose. Find out how to use paracetamol safely.
Other medicine
If your doctor gives your child ibuprofen, use it only if your child has a fever and is miserable. Don't give your child cold and flu medicines. Never give your child aspirin as this may increase the risk of Reye syndrome, which is a rare and serious illness.
Headache and other pain
If your child is in pain, as well as comforting and reassuring them, you can use medicine such as paracetamol or ibuprofen. You can buy these from a pharmacy, or ask your doctor for a prescription. If you buy it from a pharmacy, tell the pharmacist who you are getting it for to make sure that you get the right type for the age of your child. You must follow the dosage instructions on the bottle. It is dangerous to give more than the recommended dose.
Cough
Most coughs do not require treatment and get better by themselves within 3–4 weeks. Make sure your child is not exposed to any cigarette smoke.
Note the following.
Cough medicines are not useful: Cough medicines are not useful for treating cough in children.
Honey may be helpful: Honey may be helpful for a cough due to COVID-19. But, wait until your baby is at least 12 months old before giving them honey – it can make young babies sick.
Antibiotics don't help coughing caused by a viral infection: Antibiotics are not helpful for a cough caused by a viral infection. But, if your doctor finds that your child's cough is due to a bacterial infection in the throat or the chest, they may prescribe antibiotics.
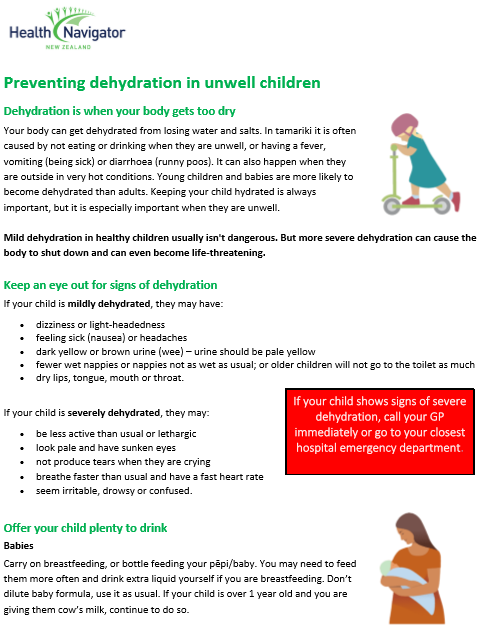
Vomiting and diarrhoea
The main treatment is to keep giving your child fluids. Whichever fluids your child is having, the important thing is to:
- offer small amounts of fluid often rather than giving large amounts - aim for a quarter of a cup every 15 minutes or 1 teaspoon or 5 mls in a syringe every minute
- keep offering your child fluids even if they are vomiting.
Types of fluids
- If you are breastfeeding, continue to feed on demand - you may need to feed more frequently and drink extra fluid yourself.
- If your child is on formula, continue to give them formula feeds.
- If your child is over 1 year, you may give them cow's milk.
- Your doctor or pharmacist may prescribe electrolyte solutions such as Electral or Pedialyte if your child is dehydrated. You can buy also electrolyte solutions from your pharmacist for approximately $15 per day.
You may also give your child the following drinks as long as they are not dehydrated. You must dilute the drinks with water as they contain too much sugar (which can make the diarrhoea worse).
- Apple juice – mix 1 part juice to 1 part water
- Cordial – make up to normal drinking strength then add 1 part of water to 1 part of cordial
- Soup – add 1 part of water to 1 part of soup
- Fizzy drinks such as lemonade – add 1 part of warm water to 1 part of drink (warm water removes the bubbles).
What drinks should I avoid giving my child with vomiting and diarrhoea?
Do not give infants or children with diarrhoea:
- undiluted soft drinks, fruit juices, Lucozade, Ribena, sports drinks (such as Powerade or Gatorade) – these contain too much sugar and can make your child's diarrhoea worse
- coffee and tea – these can make your child dehydrated.
Should I keep giving my child their normal food if they have vomiting and diarrhoea?
- You can offer your child food if they are hungry, even if their diarrhoea continues.
- Continuing to feed your child can speed up recovery and can reduce the length of time your child has diarrhoea.
- Your child may refuse food at first – this is not a problem as long as they keep taking fluids.
- If possible, do not stop giving food for more than 24 hours.
- Starchy simple foods are best – try and offer foods such as bread or toast, porridge, rice, potatoes, plain biscuits, yoghurt, milk pudding.
What foods should I avoid giving my child with vomiting and diarrhoea?
Do not give your child fatty or sugary foods such as:
- takeaways
- chippies, sweets, cakes, chocolate, ice cream, cream, coconut cream.
Will my child need any medicines for vomiting and diarrhoea?
Do not give your child medicines to reduce diarrhoea as they can be harmful in children. Your doctor may occasionally prescribe a medicine for vomiting. Follow your doctor's instructions.
A virus is usually the cause of vomiting and diarrhoea. You cannot treat viral gastro with antibiotics. The body will clear out the virus on its own without treatment.
What can I do for my baby's sore bottom from diarrhoea?
Diarrhoea can cause a rash. After each bowel motion wash your child’s bottom and pat dry. Then put on a protective cream or ointment (such as zinc and castor oil cream or Vaseline).
Resources
COVID-19 positive – stop the spread [PDF, 193 KB] Healthify He Puna Waiora, NZ, 2021
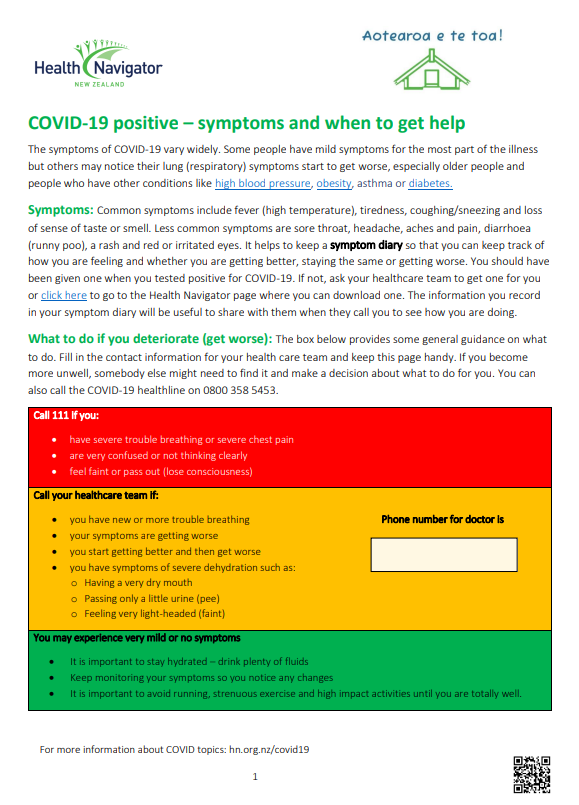
COVID-19 positive – symptoms and when to get help [PDF, 151 KB] Healthify He Puna Waiora, NZ, 2021
Preventing dehydration in unwell children [PDF, 192 KB] Healthify He Puna Waiora, NZ, 2022
Brochures
Healthify He Puna Waiora, NZ, 2021
Healthify He Puna Waiora, NZ, 2021
Healthify He Puna Waiora, NZ, 2022
Credits: Content shared between HealthInfo Canterbury, KidsHealth and Healthify He Puna Waiora as part of a National Health Content Hub Collaborative.
Page last updated:





