Bowel cancer | Mate pukupuku i te whēkau
Also known as colon, rectal or colorectal cancer
Key points about bowel cancer
- Bowel cancer (mate pukupuku i te whēkau) is any cancer that starts in your large bowel (colon), rectum (back passage) or anus.
- If it's found early it can be successfully treated.
- The 3 main symptoms of bowel cancer are blood in your bowel motions (poo), an ongoing change in bowel habits and general abdominal discomfort (frequent gas, bloating or cramps).
- Other symptoms include unexplained weight loss, tiredness and anaemia.
- These symptoms can be caused by other conditions but it's important you talk to your healthcare provider about them.

Cancer occurs when cells within a certain part of the body divide and multiply too rapidly, producing a lump of tissue known as a tumour. In bowel cancer, this occurs in the colon, rectum or anus.
Bowel cancer often starts as small, non-cancerous polyps that form on the walls of the large intestine (bowel). Polyps become more common as we get older and most are not harmful (cancerous). One type of polyp called an adenoma can become cancerous (malignant). If undetected, the cells of the polyp will multiply to form a tumour in the bowel. Read more about bowel polyps.
Anyone can get bowel cancer at any age, but certain factors make you more likely to develop it, including:
- Being over the age of 50 years.
- Having a family history of bowel cancer – especially if you have a close family member who has been diagnosed with bowel cancer at a young age (under 55 years).
- Lifestyle factors, such as:
- a diet high in red and processed meat and animal fats
- a diet low in fruit and vegetable fibre
- smoking
- drinking large amounts of alcohol
- lack of exercise
- obesity or being overweight.
- Having an inflammatory bowel condition, such as Crohn’s disease or ulcerative colitis.
- Having a rare inherited condition, known as polyposis that can lead to bowel cancer. Read more about polyposis(external link) from the NZ Familial GI Cancer Service.
- Being diagnosed with bowel cancer in the past.
Symptoms of bowel cancer may include:
- Bleeding from your bottom or blood in your poo. This may look like dark or black poo, but it can also be quite red and fresh looking depending on how far from your back passage the bleeding has occurred.
- A change in bowel habits that continues for several weeks, such as diarrhoea (runny poo), constipation (hard poo that’s difficult to pass) or feeling that your bowel doesn't empty completely.
- Severe pain in your tummy (abdomen, puku) all the time or now and again.
- Pain in your anus (bottom).
Other signs and symptoms include:
- weight loss for no obvious reason and without trying
- tiredness that's not helped with rest/sleep
- anaemia – low iron levels in your blood
- a lump in your tummy area (abdomen, puku).
Although these symptoms are often caused by other conditions, it's important to check them with your healthcare provider without delay.
When you see your healthcare provider, they’ll ask about your symptoms and whether you have a family history of bowel cancer. They may carry out some or all of the following tests and procedures to check for bowel cancer.
Rectal and abdominal examination
During this examination, your healthcare provider inserts a gloved finger into your bottom to feel for any lumps, swelling or bleeding. They will also gently feel the surface of your tummy to check for anything abnormal. These tests can be uncomfortable, and many people find the rectal examination embarrassing; however, they take less than a minute to do.
Blood tests
- You may need a blood test to check your blood cells including checking for anaemia (low red blood cells).
- A test for blood in your poo that’s used by the National Bowel Screening Programme is a faecal immunochemical test (FIT). It can detect tiny traces of blood present in a small sample of your bowel motion (poo). This may be an early warning sign that something is wrong with your bowel. A small amount of blood in your bowel motion can be caused by polyps (growths) or other minor conditions such as haemorrhoids (piles), which can easily be treated. Further investigation (usually a colonoscopy) is required to find the cause of bleeding.
Other tests
If your healthcare provider can confidently rule out other causes (eg, piles following a rectal examination), and you're experiencing symptoms of concern, you should be referred to your local hospital for further investigations.
These could include:
- A sigmoidoscopy: The doctor examines your rectum and the lower part of your bowel using a short tube (usually straight but may be flexible) called a sigmoidoscope. The doctor may also take a biopsy (a small sample of tissue).
- A colonoscopy: The doctor or nurse inspects the entire length of your large bowel by gently inserting a long, flexible tube with a video camera in it called a colonoscope. This is passed through your anus and rectum into your colon. A sedative may be given before the colonoscopy.
- Removing polyps at colonoscopy: If any polyps or other pre-cancerous lesions are found on the lining of your colon or rectum, your surgeon or gastroenterologist will remove them during the colonoscopy. A border of healthy tissue will also be removed. This is called a 'local resection'.
The polyps will be sent to a lab for analysis and if any cancer cells are found within them, your surgeon may decide you need a second, larger operation. This is to remove any cells that may have been left behind and to make sure that the cancer is unlikely to come back. - CT colonography (also known as virtual colonoscopy): This X-ray technique is increasingly replacing barium enemas. The colon is emptied with a laxative. Air is then gently pumped into your bowel via your anus. CT scans are taken of your abdomen. If abnormalities are found, then this would usually lead on to a colonoscopy.
Read more about tests and investigations for bowel cancer(external link).
The treatments for bowel cancer include chemotherapy, immunotherapy, surgery and radiation treatment. The type of treatment depends on the size of the cancer, its location and whether it has spread. You may hear these talked about as the stage of the cancer and the grade of the cancer. Read more about staging and grading.(external link)
Your general health and your wishes are also important in the decision making. In some cases you may want to seek a second opinion. Read more about getting a second opinion.(external link)
Chemotherapy and immunotherapy are often recommended as part of a treatment plan. They may have side effects but, if they’re recommended, it generally means the benefits are likely to outweigh the adverse effects. Read more about chemotherapy and targeted therapies for bowel cancer(external link).
Note: Some medicines for treating bowel cancer are fully funded in Aotearoa New Zealand but others are not. You may be offered participation in a clinical trial. Read more about unfunded medicines and clinical trials.(external link)
If bowel cancer is detected early, there’s a good chance it can be treated successfully. However, a complete cure is not always possible and the cancer may return.
If the cancer is advanced and has spread to other part of your body (also called secondary or metastatic cancer), you will be offered different treatment options. Read more about advanced bowel cancer(external link).
The links above lead to more detailed information provided by Bowel Cancer NZ.
There are some factors that increase your risk of bowel cancer that you can't change, eg, your family history and age. However, there are other factors to do with your lifestyle which you can change and by doing so reduce your chance of developing bowel cancer.
Lifestyle factors
There's strong evidence that certain lifestyle factors contribute to our risk of bowel and other cancers. To lower your risk it's recommended that you:
- adopt a healthy diet that includes:
- less cured and processed meat, eg, bacon, sausages and ham
- less red meat and more fish
- more fibre from cereals, beans, fruit and vegetables.
- exercise regularly:
- for adults, that’s at least 2.5 hours of moderate intensity activity every week.
- maintain a healthy weight:
- it's particularly important to be aware of the amount of weight you carry around your middle – your waist to hip difference. (external link)
- changes to your diet and an increase in your physical activity will help keep your weight under control.
- quit smoking
- cut back on alcohol.
Read more about bowel cancer prevention(external link) from Bowel Cancer NZ.
Early detection
Bowel cancer is the second highest cause of death due to cancer in Aotearoa New Zealand. When detected early, it can be successfully treated.
Bowel screening cannot prevent bowel cancer, but it can help the condition to be detected earlier. People who are diagnosed with bowel cancer and receive treatment at an early stage, have a more than 90% chance of long-term survival. If there's a delay in diagnosis and treatment, the cancer can become more advanced and harder to cure.
Bowel screening is available every 2 years for people aged 60–74 years who are eligible for publicly funded health care. Read more about bowel cancer screening.(external link)
Video series interviewing people about their personal journey with bowel cancer including the signs, symptoms and treatment. These videos may take a few moments to load.
Video: Chelsea's story
(Bowel Cancer, NZ, 2018)
Video: Jonny's story
(Bowel Cancer, NZ, 2018)
For more personal stories in the same series visit Bowel Cancer NZ(external link).
Emotions and cancer English/te reo Māori(external link) Cancer Society, NZ
We're here for you(external link) Bowel Cancer NZ
How we can help?(external link) Cancer Society, NZ
NZ cancer services – find a hospital/service near you(external link) Healthpoint, NZ
Support services
There's a wide range of services and support for people and families living with cancer at all stages of the journey.
Bowel Cancer NZ
Bowel Cancer NZ(external link) provides nationwide, accessible patient support from diagnosis onwards. So if you or a loved one is going through or just completed treatment, Bowel Cancer NZ provides:
- free counselling (for you and close whānau – including your primary caregiver and children)
- funded physiotherapy
- financial assistance
- online support groups
- free nurse helpline
- bowel cancer specific resources.
To learn more, please visit Bowel Cancer NZ support(external link) or call 0800 BCNZ NURSE (226 968).
Cancer Society of NZ
To find courses and support groups near you, call the Cancer Society of NZ(external link) cancer information helpline 0800 CANCER (226 237). The helpline is staffed by nurses and provides a wide range of services from telephone support to booklets, pamphlets, DVDs and signposting to credible internet sites, including:
- CanTalk – online magazine.
- Information about services in your area.
- The range of support groups, programmes, workshops, seminars and online forum available.
- A range of supports from help with transport, accommodation to limited financial assistance during treatment.
Other people's experiences
To hear about other people who may have had a similar experience to you see the personal stories(external link) section on the Bowel Cancer New Zealand website.
About bowel cancer(external link) Beat Bowel Cancer Aotearoa, NZ
Brief information about bowel cancer(external link) Cancer Society, NZ
Brochures
Bowel cancer – a guide for people with bowel cancer(external link) Cancer Society NZ, 2018
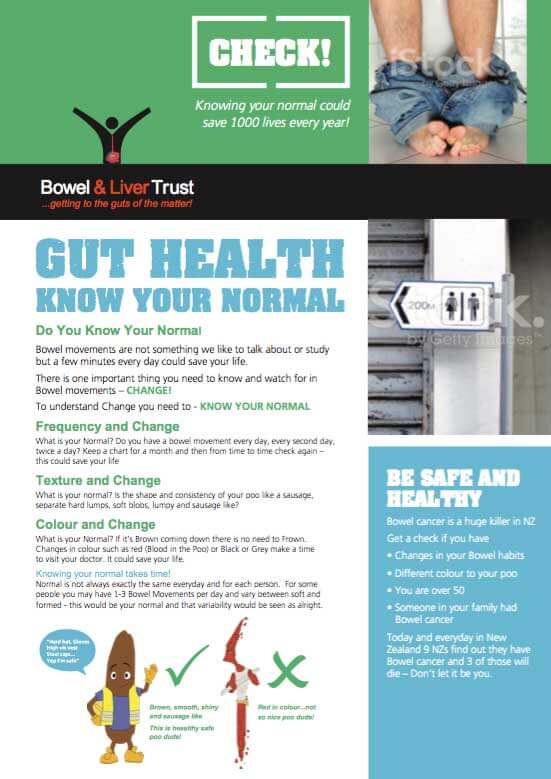
Gut health – know your normal [PDF, 351 KB] Gut Foundation, NZ
Supporting someone with cancer [PDF, 3 MB] Cancer Society, NZ, 2015
Living with cancer resources(external link) Cancer Society NZ
Telling others about your diagnosis(external link) Cancer Society, NZ, 2019
Side effects – constipation, diarrhoea and wind(external link) Cancer Society, NZ, 2019
Side effects of cancer treatment – eating and mouth problems(external link) Cancer Society, NZ, 2020 English(external link), te reo Māori(external link)
Coping with fever and nausea(external link) Cancer Society, NZ, 2019
Managing cancer pain(external link) Cancer Society, NZ, 2020
References
About bowel cancer(external link) Bowel Cancer NZ
Clinical guidelines and resources
Referral of patients with features suggestive of bowel cancer – Ministry of Health guidance(external link)(external link) BPAC, NZ, 2021
Surveillance for people with polyps or inflammatory bowel disease(external link)(external link) BPAC, NZ, 2021
Follow-up and surveillance for people after treatment for bowel cancer(external link)(external link) BPAC, NZ, 2021
Management of early colorectal cancer(external link)(external link) NZ Guidelines Group, Ministry of Health, NZ
Management of early colorectal cancer – pocket summary(external link)(external link) Ministry of Health, NZ, 2011
Colorectal cancer presenter slide set – oncology(zip, 5.5 MB)(external link)(external link) NZ Guidelines Group, Ministry of Health, NZ
Prioritising primary care patients with unexpected weight loss for cancer investigation – diagnostic accuracy study(external link)(external link) The BMJ, UK, 2020
Resources for clinicians on the national bowel screening programme
Referral of patients with features suggestive of bowel cancer – Ministry of Health guidance(external link)(external link) BPAC, NZ, 2020
National bowel screening programme for health professionals(external link)(external link) National Screening Unit, NZ, 2017
Quick reference guide for primary healthcare teams(external link)(external link) National Screening Unit, NZ, 2018
National bowel screening programme(external link) Time to screen
Final Evaluation Report of the Bowel Screening Pilot Screening Rounds One and Two(external link) Ministry of Health, NZ
Serious illness conversation guide Aotearoa(external link) Health Quality & Safety Commission, NZ
Blackmore T, et al. The characteristics and outcomes of patients with colorectal cancer in NZ, analysed by Cancer(external link)(external link) NZ Med J. 2020;133(1513):42-52.
Brochures
Cancer Society NZ, 2018
Just diagnosed with bowel cancer – what happens next?
Bowel Cancer NZ,
Gut Foundation, NZ
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Bowel Cancer NZ
Last reviewed:





