You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Asthma – first aid
What to do if someone's having an asthma attack
Key points about asthma first aid
- An asthma attack is an emergency and symptoms can get worse quickly – act fast.
- Anyone with asthma can have a severe asthma attack.
- Worsening asthma symptoms include wheeze, feeling short of breath, tightness in your chest and coughing.
- If you have an asthma action plan follow the instructions there.
- If you don't have an asthma action plan follow the instructions on this page.
- If your asthma attack doesn't get better with asthma first aid dial 111 and ask for an ambulance.

An asthma attack is when your airways swell and narrow, and make more mucus. You find it difficult to breathe, your chest can feel tight, and you might wheeze or cough.
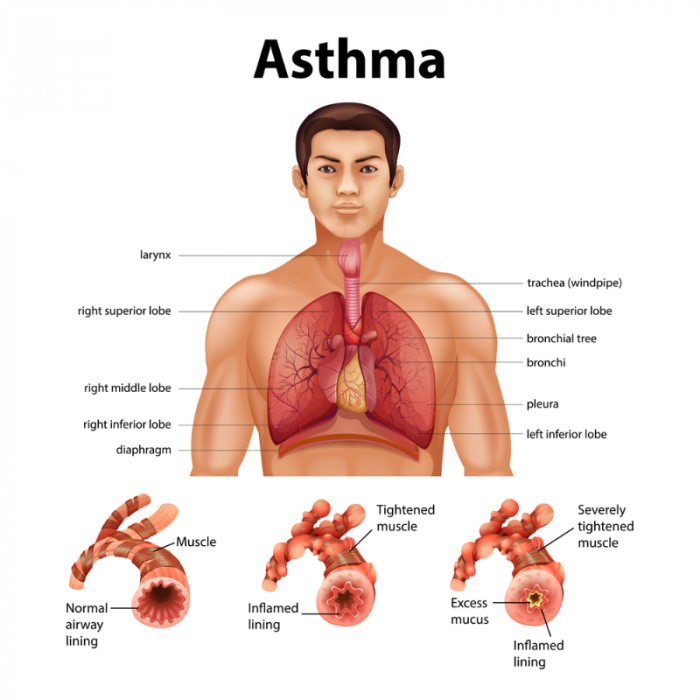
Image credit: Depositphotos
Note: The information on this page is for adults. See KidsHealth, NZ for information about asthma attacks in children(external link).
An asthma attack may be mild, moderate or severe
- Anyone with asthma can have a severe asthma attack.
- An asthma attack can take anything from a few minutes to a few days to develop.
- Symptoms may be mild or moderate and can quickly get worse so it's important to act fast.
- If you have an asthma action plan follow the instructions on there.
Mild asthma symptoms
Early signs that asthma may be getting worse can include feeling breathless, chest tightness, cough and mild wheeze especially morning and night or when you're exercising or excited.
Moderate asthma symptoms
When asthma becomes more serious, your symptoms may include:
- worse cough or wheeze
- difficulty breathing
- difficulty talking, you can only talk in short sentences
- your reliever inhaler only works for a few hours.
Severe symptoms – call 111 if:
- you're gasping for breath
- you can't speak a full sentence in 1 breath
- you're blue around the mouth
- you've used a reliever inhaler but it's not helping much.
If you or someone near you is having an asthma attack, follow the ASTHMA acronym. Someone having an asthma attack may not be able to follow asthma first aid themselves – they are relying on you to help.
A = Assess
Assess whether the person's asthma attack is mild, moderate or severe.
If the person has severe asthma or is frightened, call an ambulance on 111.
S = Sit
Sit the person upright and stay with them. Reassure them calmly.
T = Treat (with a reliever inhaler)
It's important to carry your reliever inhaler with you at all times. If you're helping someone else you may need to help them find one.
- Symbicort or DuoResp Spiromax: Use 1 puff initially and repeat if needed, up to 12 puffs daily. These inhalers quickly reduce inflammation of your airways and help you to breathe more easily.
- Ventolin or SalAir: Always use a spacer with these inhalers. Inhale 1 puff through the spacer and take 6 breaths per puff. Use 1 puff initially and repeat if needed, up to 6 puffs. For severe symptoms, use 6 puffs through the spacer, every 6 minutes until help arrives. Make sure to take 6 slow breaths for each puff.
- Bricanyl: Use 1 puff initially and repeat if needed, up to 6 puffs.
H = Help
If the person is not improving, call an ambulance immediately on 111. Continue to use the reliever inhaler every few minutes until help arrives.
M = Monitor
- If the person is improving, keep monitoring them for signs of improvement or worsening of symptoms. If necessary, repeat doses of the reliever inhaler.
- If the person is not improving, continue to use the reliever inhaler every few minutes until help arrives.
A = All OK!
When the person is free of wheeze, cough or breathlessness, they can return to quiet activity.
Make sure a preventer inhaler is part of your asthma management plan. This is important to reduce the chance of this type of attack happening. This may mean a separate preventer inhaler is needed, or a combined reliever and preventer inhaler if you don't have this already.
Make sure an asthma action plan is written up to guide you through asthma attacks in the future. Regular peak flow monitoring may be useful to reduce the chance of further asthma attacks. Read more about peak flow monitoring.
If symptoms come back, repeat the treatment and rest. It's always important to see your healthcare provider as soon as possible after an asthma attack.
Video: What to do in an asthma emergency (1:23)
Action plans
4-stage asthma action plans(external link) Asthma Foundation, NZ, English(external link), te reo Māori(external link), Samoan(external link), Tongan(external link), Simplified Chinese(external link)
Brochures
Asthma – first aid poster (external link)Asthma and Respiratory Foundation NZ English(external link), te reo Māori(external link)
GINA patient guide for asthma – you can control your asthma(external link) Asthma and Respiratory Foundation NZ
Summer holiday asthma and allergies checklist(external link) Asthma and Respiratory Foundation NZ
Asthma checklist(external link) Asthma and Respiratory Foundation NZ
Allergy and asthma fact sheet(external link) Asthma and Respiratory Foundation NZ
Breathing and asthma(external link) Asthma and Respiratory Foundation NZ
Apps
References
- Asthma first aid(external link) Asthma and Respiratory Foundation NZ
- What to do in an asthma emergency(external link) Asthma New Zealand
- NZ adolescent and adult asthma guidelines(external link) NZ Respiratory Guidelines, NZ, 2020
Algorithm for management of acute severe asthma in adolescents and adults(external link) Asthma Foundation, NZ
NZ Adolescent and Adult Asthma Guidelines(external link) Asthma Foundation, NZ, 2020
See our page Asthma in adults for healthcare providers, Long-term conditions for healthcare providers
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Emma Dunning, Clinical Editor and Advisor
Last reviewed:





