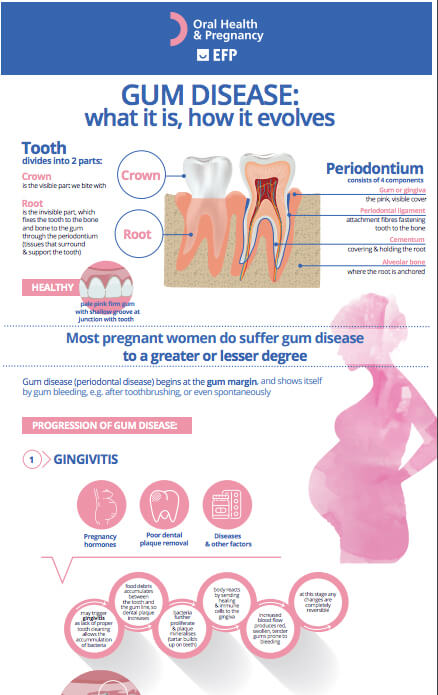
Any of the symptoms may be a sign of a serious problem, which should be checked by a dentist. The main goal of treatment is to control the bacteria and the infection. The number and types of treatment will vary, depending on the extent of the disease. With any treatment, you will need to keep up good daily oral care at home. If you smoke, your dentist may suggest you quit to improve the outcome of the treatment.
Scaling and root planing
As gum disease progresses, plaque forms below your gum line in the pockets that have formed. This is impossible for you to clean off by yourself. Instead, a dentist, periodontist, or dental hygienist can remove the plaque through a deep-cleaning method called scaling and root planing.
Scaling means scraping off the plaque from above and below your gum line. It is a deep clean of all the hard and soft deposits on your teeth. Root planing gets rid of rough spots on the tooth root where bacteria gather and helps remove bacteria that contribute to the disease.
Laser treatment
In some cases, a laser may be used to remove plaque and tartar. This procedure can result in less bleeding, swelling and discomfort.
Medication
Medicines may be used with treatment that includes scaling and root planing, but they can't always take the place of surgery. Depending on how far the disease has progressed, the dentist or periodontist may still suggest surgical treatment. Long-term studies are needed to find out if using medicines reduces the need for surgery and whether they're effective over a long period of time.
Talk to your dentist or periodontist about whether any mouthwashes, antibiotics or other medication would help in your case.
Flap surgery
Surgery might be necessary if inflammation and deep pockets remain following treatment with deep cleaning and medications.
This common surgery involves lifting back your gums and thoroughly removing the tartar. The gums are then stitiched back in place so that the tissue fits snugly around the tooth again. This makes it easier to keep the area clean. After surgery, the gums will heal and fit more tightly around the tooth. This sometimes results in the teeth appearing longer. While this sounds extreme, it can often be the best way to completely clear the pockets and clean the surfaces, with better healing in the long term.