Glaucoma | Mate pēhinga karu
Key points about glaucoma
- Glaucoma (mate pēhinga karu or papahewa) is an eye disease that causes damage to your optic nerve.
- If it’s not treated in time, it can result in blindness, so early detection is very important.
- More than 1 in 10 people over the age of 80 have glaucoma.
- Often there are no symptoms, so it's important to get regular eye checks from 45 years of age.
- If you have glaucoma, treatments are available that can prevent significant loss of vision.
- Get medical help urgently if you experience sudden vision changes or eye pain.

Glaucoma is an eye disease that causes damage to the optic nerve in your eye (the nerve that connects the eye to the brain). Pressure from fluid in your eye (intraocular pressure) can build up and this is what damages the optic nerve.
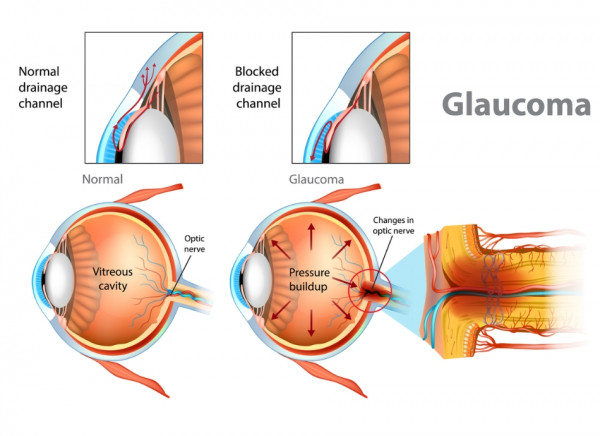
Image credit: Depositphotos
It’s sometimes called the ‘silent thief of sight’ because you can slowly lose your vision without being aware of it. That’s why it’s important to have regular eye health examinations by an eye health professional – an optometrist or ophthalmologist.
Glaucoma is one of the most common causes of preventable blindness in Aotearoa New Zealand and some types can be inherited (run in families). Glaucoma can’t be cured, but if it’s found early, treatment can stop it progressing and stop you from losing your sight.
There are different types. The most common type of glaucoma is chronic open-angle glaucoma. Acute angle closure glaucoma is an emergency as vision loss and blindness can occur quickly.
In the video below, glaucoma specialist Dr Divya Perumal talks about how glaucoma is diagnosed and managed.
Video: An introduction to glaucoma
(Glaucoma New Zealand, NZ, 2019)
How does glaucoma cause vision loss?
Fluid is produced in the front of your eye and this fluid produces pressure in your eye. Anything that slows or blocks the flow of this fluid will cause the pressure in the eye to increase and this pressure can eventually lead to optic nerve damage. The optic nerve is the ‘cable’ that connects your eye to your brain. It’s the nerve that sends images from your eye to your brain, so damage to this nerve causes loss of vision.
The damage to the optic nerve can’t be reversed so glaucoma must be found early to stop the damage getting worse.
For some people, damage to the optic nerve can occur when the eye pressure is in the normal range (normal tension glaucoma). In these cases, the damage is thought to be due to pressure sensitivity.
Most types of glaucoma develop slowly so you may not have any symptoms early on. Depending on the type, you may experience a ‘jack in the box’ perception of the sudden presence of objects missed from your peripheral vision, or have blurry, misty patches in your vision.
When to seek urgent medical help
In cases of acute angle-closure glaucoma and some other causes of glaucoma, you may develop sudden onset of these symptoms:
- blurred vision
- seeing coloured halos around lights
- redness of your eye
- nausea or vomiting
- pain in your eye.
These are all serious symptoms, and you should see a doctor immediately.
There are different types of glaucoma that can cause different symptoms and need different treatments.
Open-angle glaucoma
- This is the most common type of glaucoma. The cause is unknown.
- Damage to the optic nerve develops slowly and causes blind spots in your vision, but there are usually no symptoms early on.
- The actual pressure in the eye that damages the optic nerve varies from person to person.
- This type of glaucoma can run in families, so you are at greater risk if you have a parent, brother or sister with open-angle glaucoma.
- The risk also increases over the age of 40.
- Treatment will stop vision loss getting worse, however, it won’t restore vision that has already been lost.
Angle-closure glaucoma
- Acute angle-closure glaucoma is a medical emergency.
- It happens when there is a sudden complete blockage of the fluid in your eye, which causes a rapid increase in eye pressure.
- It may occur after you’ve been given dilating eye drops or certain other medicines (eg, medications which treat seizure, migraine, depression and nausea).
Contact your eye health professional urgently if you suddenly develop eye pain, blurred vision, haloes around lights, and nausea and vomiting.
Secondary glaucoma
- This is glaucoma that happens due to a known cause.
- Causes of secondary glaucoma include use of steroid medicines, certain eye diseases (eg, uveitis, which is inflammation of the middle layer of the eye), diabetes or eye injury.
Congenital glaucoma
- This type of glaucoma occurs in babies when the eye doesn’t develop normally.
- It’s present at birth and can run in families.
Glaucoma with normal pressure
- In this type of glaucoma, there is damage to the optic nerve without the eye pressure being above the normal range.
Your risk of glaucoma is greater if you:
- are over 40 years of age
- have a family history of glaucoma
- are either short-sighted or long-sighted
- have a history of migraine or Raynauds syndrome
- used steroid medicines
- have had a previous eye injury
- have diabetes
- have high blood pressure.
If any of these apply to you, get an eye check from an optometrist or ophthalmologist at least every 1 to 2 years.
An optometrist is a health professional who is trained to detect and manage eye problems. An ophthalmologist is a doctor who specialises in the health of the eye and may also perform glaucoma surgery.
If you have glaucoma, you should tell your family about the condition and encourage them to get tested regularly from the age of 25.

Image credit: Canva
You can’t prevent glaucoma, but early detection through regular eye check-ups is the key to protecting your vision from damage caused by glaucoma. Glaucoma is easy to treat when found early.
- If you are in any of the higher risk groups above, have an eye check at least every 1 to 2 years.
- For everyone else, have a regular eye check from the age of 45 (see the 45 + 5 recommendations below).
- If you are over 60 years of age, get your eyes checked every year.
The 45 + 5 eye examination
If you have glaucoma, tell you whānau about the condition and encourage them to get tested regularly from the age of 25.
Glaucoma NZ(external link) recommends the 45 + 5 glaucoma eye examination if you don’t have any risk factors for glaucoma.
- From the 45 years of age, have an eye check examination with an eye health professional – even if you haven’t had any eye problems.
- If the examination is normal, you can repeat it every 5 years.
- If the examination shows any signs of glaucoma, your eye specialist will advise you on a course of treatment.
For most types of glaucoma, the only way you can tell if you have the condition is through an eye test done by an optometrist. Early detection is the key to protecting your vision from damage caused by glaucoma.
A complete eye exam by your eye health professional will include several tests to detect glaucoma.
Common tests include taking measurements of:
- your vision
- your inner eye pressure (intraocular pressure)
- the appearance of the optic nerve
- your field of vision (this indicates the function of the optic nerve)
- the drainage angle (where fluid drains out of your eye)
- the thickness of your cornea
- the structure of your optic nerve and retina.
If your optometrist finds that you have glaucoma they will refer you to an ophthalmologist (a medical eye doctor) for further assessment and treatment.
The most important thing to do if you have glaucoma is to go to all of your regular appointments and follow the instructions given to you by your eye health professional. Ask them how often you should have check-ups and stick to that schedule.
Know the names of your medicines and how often you need to use them. Taking your medicines as instructed is extremely important. Not taking glaucoma medication is a major cause of blindness in people with glaucoma.
Call your healthcare provider if you have any unusual symptoms or eye problems.
Tell your whānau members about your glaucoma and suggest that they have an eye check-up as it often runs in families.
Slowing the progression
The following are things you can do to that may slow the progression of glaucoma.
- Avoid smoking.
- Do regular aerobic exercise, eg, walking, jogging, cycling.
- Eat a balanced diet – try to include lots of green leafy vegetables, carrots, broccoli, cauliflower, cabbage, berries and citrus fruits. These foods contain antioxidants or nitrates which may reduce your risk of glaucoma.
- Maintain a healthy cholesterol level – you may need to alter your diet or take cholesterol-lowering medication if your cholesterol is high.
- Avoid headstand positions (eg, if doing yoga).
- Be cautious about playing wind instruments, eg, a trumpet, trombone or bagpipes – especially if you have advanced glaucoma
- Maintain a healthy blood pressure.
- Avoid drinking lots of water too quickly – eye pressure can increase if you drink more than 0.5 to 1 litre of water over a short period (5 to 15 minutes).
- Don’t drink more than 2 cups of caffeinated coffee a day.
- If you drink alcohol, do so in moderation.
- If you wear neck ties don’t have them too tight.
- See a healthcare provider if you have sleep apnoea as this condition is associated with glaucoma.
Here’s some advice on travelling with glaucoma(external link). Put your eye drops in your hand luggage when travelling.
Can I drive if I have glaucoma?
Having glaucoma doesn’t necessarily mean you can’t drive any more.
Depending on how bad it is, you may still be able to drive as long as you keep track of your eyesight, regularly assess your driving and practise good road safety.
Ask yourself these questions:
- Do other cars sometimes seem to come out of nowhere?
- Do other drivers often honk at you?
- Do you feel uncomfortable driving at night?
- Does the glare of oncoming headlights bother you?
- Do you find it hard to park your vehicle?
- Do you feel anxious or stressed when driving?
If you answered yes to any of these questions, it might be a sign that your eyesight is affecting your driving. Ask your eye health professional for advice.
Video
Glaucoma and driving Glaucoma specialist Dr Hussain Patel discusses how living with glaucoma affects driving and how different driving conditions can prove difficult and why.
Apps reviewed by Healthify
You may find it useful to look at some Vision difficulty apps.
Although glaucoma can’t be cured, treatment can be given to stop it from getting worse.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these.
If you have had an acute glaucoma attack in 1 eye, you’re at risk of having an attack in your other eye so your eye specialist is likely to also treat your second eye to prevent an attacking happening in that eye.
Treatment of secondary glaucoma depends on the cause. The aim of treatment is to try and bring your eye pressure down into the normal range to slow down any further damage to the optic nerve.
Congenital glaucoma is mostly treated with surgery.
Eye drops
Eye drops are the most commonly used treatment. They reduce the pressure in your eye by helping the fluid drain from your eye or by reducing the amount of fluid produced. You may need more than one type of eye drops. Read more about eye drops for glaucoma.
Laser treatment
Laser treatment can make it easier for fluid to drain from your eye. The lasers used for glaucoma are different from the laser surgery used to correct vision. The types of laser treatment for glaucoma include:
- Laser trabeculoplasty: This is a safe, easy treatment for most people with glaucoma. Read more about laser trabeculoplasty(external link).
- Laser iridotomy and laser iridoplasty: This treatment is most often used if you have narrow angle or angle-closure glaucoma. Read more about laser iridotomy(external link).
Surgery
If you have progressive glaucoma, despite medical and laser therapy, or if you have significant side effects from medical therapy, surgery may be the only form of treatment for controlling the pressure in your eyes.
Most surgeries are day procedures, which means you don't need to stay in hospital after the procedure. The procedures can range between 10 to 90 minutes and may be done together with cataract surgery. Most procedures are done under local anaesthetic.
Surgical options include the following:
- Filtration surgery (trabeculectomy and deep sclerectomy).
- Putting in a drainage tube (Paul, Molteno, Ahmed, Baerveldt).
- Cyclodiode laser.
- Minimally invasive glaucoma surgery (MIGS), eg, iStent, Hydrus, Goniotomy, Xen, Preserflo, GATT, Micropulse devices.
You can find out more about these surgical options in the section below.
Filtration surgery (trabeculectomy and deep sclerectomy)
- This is the traditional glaucoma operation that has been performed for 40+ years. It involves making a separate channel for the fluid to drain out of your eye.
- Follow-up after glaucoma surgery is fairly frequent at first, and can include weekly reviews for the first 6 weeks.
- In these reviews, small adjustments are performed in the clinic and may include injections.
- You may need to be off work for up to 2 weeks after your procedure, depending on your vision and how strenuous your work is. Your ability to drive and perform lifting may be affected during your recovery period. Consult your surgeon as to when you can best return back to normal function.
- Potential risks of surgery include high or low eye pressure, damage to your cornea, inflammation, reduced vision and bleeding.
Drainage tube
- This procedure involves placing a silicone tube into the front of your eye, which allows fluid to drain out onto a plastic plate that’s been secured to the wall of the eye.
- This procedure is generally used for advanced glaucoma and refractory glaucoma (glaucoma that hasn’t responded to previous surgery).
- It’s generally performed under general anaesthesia or local anaesthesia with sedation and usually takes up to 90 minutes.
- Potential risks include damage to your cornea, cataract, exposure of the implant, high eye pressure, low eye pressure, double vision and reduced vision.
Cyclodiode laser
- This procedure involves applying a special laser treatment though the coat of your eye, which targets reducing the production of aqueous.
- It is usually done under local anaesthetic and takes about 15 minutes.
- Potential risks include failure to sufficiently reduce eye pressure, inflammation and shrinking of your eye.
Minimally invasive glaucoma surgery (MIGS)
This refers to a group of glaucoma surgeries that use smaller incisions and generally have a safer and quicker recovery. Surgeons trained in performing glaucoma surgery conduct additional training in the use of these devices. MIGS procedures are effective and have fewer side effects compared to traditional glaucoma treatment.
- MIGS devices in Aotearoa New Zealand include iStent, Goniotomy, Hydrus, Xen, Preserflo and micropulse.
- MIGS procedures can improve glaucoma control or may reduce the need for eye-drops.
- Access to MIGS devices for the management of glaucoma is available in most public hospitals in Aotearoa New Zealand, and is covered by most insurance companies.
MIGS procedures may be particularly beneficial if you:
- can't tolerate eye drops because of side effects or allergy
- can't use eye drops for other health reasons
- are having a cataract operation and have mild to moderate glaucoma, and would like to decrease the number of drops you’re using.
Surgery videos
- Glaucoma and surgery(external link) Glaucoma specialist Dr Divya Perumal discusses the benefits and risks associated with the different types of glaucoma surgeries currently available and how they work.
- Latest advances in glaucoma surgery(external link) Dr Perumal discusses the latest advances.
Video: Understanding Glaucoma - Jean's story
Watch Jean tell her story and what living with sight loss means to her.
(RNIB, UK, 2017)
Video: Amanda Eddy: My Glaucoma Story
Amanda Eddy is a jewellery designer who was born with glaucoma.
(Glaucoma Research Foundation Videos, US, 2017)
Read more personal stories at Glaucoma NZ.(external link)
Glaucoma New Zealand provides information, support and education to people living with or caring for someone with glaucoma. You can contact them at [email protected] or freephone 0800 GLAUCOMA (0800 452 826). Glaucoma New Zealand membership, information and services are free.
Services
Search for an optometrist near you(external link) NZ Association of Optometrists
Search public hospital services, add your region(external link) Healthpoint NZ
Search for a private eye specialist by region(external link) Healthpoint NZ
Glaucoma section(external link) NZ Association of Optometry
Minimally invasive glaucoma surgery(external link) International Glaucoma Association
Glaucoma Australia(external link)
Glaucoma and surgery – Dr Divya Perumal(external link) Glaucoma NZ
Apps
Brochures
A range of glaucoma factsheets (external link)Glaucoma NZ
Your eyes(external link) Glaucoma NZ
Glaucoma(external link) New Zealand Association of Optometrists
Glaucoma eye examination checklist(external link) Glaucoma NZ
References
- Glaucoma(external link) NZAO
- About glaucoma (external link)Glaucoma New Zealand
- Primary glaucoma(external link) Glaucoma New Zealand
- Open-angle Glaucoma(external link) Auckland Region Community HealthPathways, NZ, 2023
- Acute angle-closure glaucoma(external link) Auckland Region Community HealthPathways, NZ, 2023
- Glaucoma(external link) MedlinePlus, US, 2022
Clinical guidelines
Glaucoma – who to refer for testing and how to manage their treatment(external link) BPAC, NZ, 2014
Glaucoma overview map(external link) NICE, UK, 2013
Continuing professional development
Video: Glaucoma and lifestyle factors – Dr Jim Stewart Glaucoma New Zealand, 2019
Video: Glaucoma and research – Professor Helen Danesh Meyer (external link)Glaucoma New Zealand, 2019
Video: Glaucoma and surgery – Dr Divya Perumal(external link) Glaucoma New Zealand, 2019
Video: The latest treatment in glaucoma – Dr Divya Perumal(external link) Glaucoma New Zealand, 2024
Apps
Brochures

Acute angle closure glaucoma
Glaucoma NZ

Lifestyle factors that may affect glaucoma
Glaucoma NZ
Your eyes
Glaucoma NZ
English, te reo Māori, Samoan, Tongan, Chinese (simplified), Chinese (traditional), Hindi, Punjabi, Japanese, Korean, French
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Divya Perumal, Ophthalmologist, Auckland
Last reviewed:





