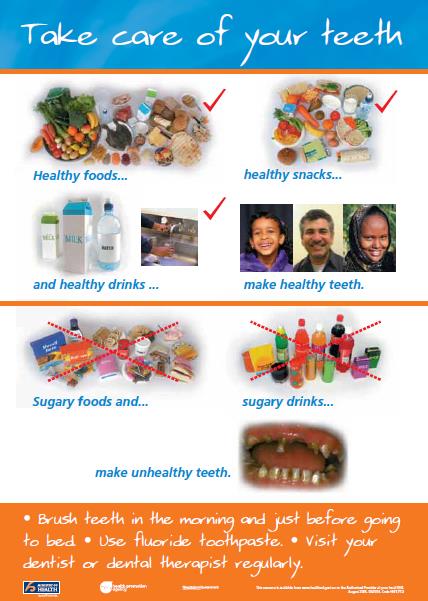
Gingivitis is a common and mild form of gum disease causing redness and swelling of the gums around the base of your teeth.

Image credit: Depositphotos
Gingivitis mostly occurs if you don’t look after your teeth properly, or if an area is often missed by your toothbrush by mistake, when cleaning your teeth. If your teeth aren’t cleaned well at home and checked regularly by a dentist, plaque can build up where your gums meet your teeth. If it’s not managed, gingivitis can lead to periodontal disease.