Cytomegalovirus (CMV)
Key points about Cytomegalovirus (CMV)
- Cytomegalovirus (CMV) is a common virus passed on through close contact with another person.
- For most people it's harmless, but it can cause serious health problems for people with weakened immune systems and for unborn babies.
- If you have weakened immunity, or if you're pregnant, and you get flu-like symptoms, see your healthcare provider.
- Most people don’t need treatment for CMV, but antiviral medicine can be used to treat people with a weakened immune system and babies.
- Limit your risk of getting CMV by following good hygiene practices.

CMV is a virus. It's mainly spread through being in close contact with someone who already has it. It can be passed on through contact with body fluids including saliva, blood, urine, semen and breast milk.
CMV can only be passed on when it is ‘active’. This is when:
- you catch the virus for the first time – young children often get CMV for the first time when they start early childhood education
- the virus has been re-activated because you have a weakened immune system
- you’ve been re-infected with a different strain (type) of CMV from what your body may have been infected with before.
Once you have it, it stays in your body for the rest of your life, but in an inactive form in most healthy people.
Most people infected with CMV show no signs or symptoms. That’s because a healthy person’s immune system usually keeps the virus from causing illness.
Some people get symptoms similar to the flu or glandular fever the first time they catch CMV, including:
- a high temperature of 38°C or more
- aching muscles
- tiredness
- feeling sick
- sore throat
- swollen glands.
If you do have symptoms, they normally get better on their own within about 3 weeks. It’s rare to get symptoms again unless your immune system becomes weakened, eg, due to organ transplant or chemotherapy. It can also be reactivated during pregnancy.
If you have a weakened immune system and get CMV, you can have more serious symptoms affecting your eyes, lungs, liver, oesophagus, stomach and intestines.
Pregnant people can pass an active CMV infection on to their unborn pēpi. This is known as congenital CMV. Pregnant people who work closely with children or already have a young family are more at risk of catching CMV.
Most babies born with CMV infection are healthy at birth and grow up with normal health. Some babies appear healthy at birth but develop problems (eg, hearing problems) later on.
A small number of babies with congenital CMV are sick at birth and have significant signs and symptoms. These include:
- premature birth
- low birth weight
- yellow skin and eyes (jaundice)
- enlarged and poorly functioning liver
- purple skin splotches or a rash or both
- abnormally small head (microencephaly)
- enlarged spleen
- pneumonia
- seizures.
In the most severe cases, congenital CMV can lead to stillbirth (your baby born dead) or neonatal death (dying after birth).
Some babies with signs of congenital CMV infection at birth may have long-term health problems, eg, hearing loss, developmental and motor delay, and vision loss.
How is CMV diagnosed?
See your healthcare provider if you have flu-like symptoms and you’re pregnant or you have a weakened immune system, eg, because of chemotherapy. If your healthcare provider is worried about your or your baby’s health they will arrange tests of your blood or other body fluids.
How is CMV treated?
If you don’t have any symptoms, CMV doesn’t need treatment. There’s currently no treatment for CMV in pregnancy and in most cases, the virus doesn’t cause problems for your baby.
Antiviral medicine can be used to treat:
- babies diagnosed with congenital CMV after they are born
- people with a weakened immune system.
The treatment aims to weaken the virus and reduce the chance of serious problems – but it doesn’t cure CMV infection.
Babies born with congenital CMV need to stay in hospital until the antiviral treatment finishes.
There’s currently no vaccine for CMV. The best way to reduce your risk of catching CMV during pregnancy is with good hygiene:
- Wash your hands using soap and hot water – especially after changing nappies, feeding young children or wiping their nose.
- Regularly wash toys or other items that get young children's saliva or urine on them.
- Avoid sharing food, cutlery, drinking glasses or dummies with young children.
Other tips include:
- Avoid contact with saliva when kissing a child.
- Don't put a pacifier (dummy) in your mouth.
- Don't share food, utensils, drinks or straws.
- Don't share a toothbrush.
- Wash your hands after changing a nappy.
The following links provide further information about CMV. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
A range of CMV resources(external link) CMV Action, UK
National CMV Foundation(external link) US organisation providing information and resources about CMV, particularly congenital CMV
Apps
Pregnancy, baby care and parenting apps
Resources
Protect your baby from CMV(external link) The Children's Hospital Westmead, Australia
CMV fact sheet for pregnant women and parents(external link) Centers for Disease Control and Prevention, US
References
- Cytomegalovirus (CMV)(external link) NHS, UK, 2023
- Cytomegalovirus (CMV) and pregnancy(external link) NSW Government Health, Australia, 2017
- Cytomegalovirus infection(external link) Department of Health and Human Services, Victoria, Australia, 2015
- Cytomegalovirus (CMV) infection(external link) Mayo Clinic, US, 2022
- About CMV(external link) Centre for Disease Control and Prevention, US, 2024
Starship Children’s hospital Cytomegalovirus (CMV)(external link) contains diagnosis and investigation information
Treatment
The recommendations for treatment of congenital CMV are evolving. Consult the paediatric infectious disease team.
Other resources
Cytomegalovirus in pregnancy NZ Maternal Fetal Medicine Network, 2016
Cytomegalovirus infection(external link) BMJ Best Practice, UK, 2024
Cytomegalovirus(external link) Patient Info Professional, UK, 2022
CMV fact sheet for healthcare providers(external link) Centers for Disease Control and Prevention, US, 2018
Apps
Brochures

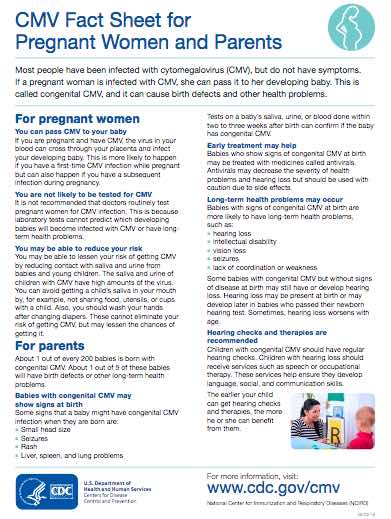
Centers for Disease Control and Prevention, US, 2018
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator.
Last reviewed:





