C. diff bacteria are found in the gut of about 1 in every 30 healthy adults. The bacteria usually live harmlessly without causing you to become ill because other bacteria normally found in your bowel keep them under control. But some antibiotics can interfere with the balance of bacteria, which can cause the C. diff bacteria to multiply and produce toxins (poisons). This causes diarrhoea (runny poo) and makes you feel unwell.
C. diff can spread easily to other people because the bacteria are passed out of your body in your diarrhoea. If you have a C. diff infection you are generally considered to be infectious (able to pass the infection to others) until at least 48 hours after your symptoms have cleared up.
Love our website? We do too. Did you know we're a charity? Donate now to help us keep it free for everyone in Aotearoa New Zealand.
Clostridium difficile infection
Also called C. diff or Clostridioides difficile infection
Key points about clostridium difficile infection
- Clostridium difficile (sometimes called 'C. diff') is a type of bacteria that can cause infection in your gut.
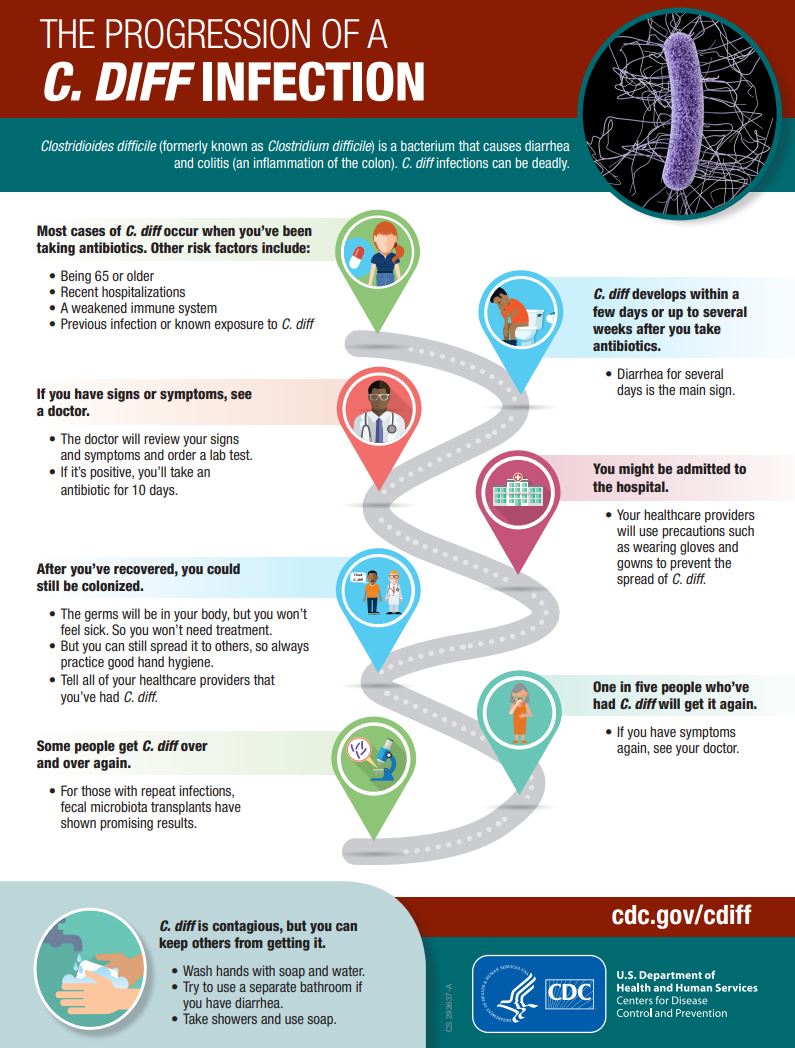
- Infection with Clostridium difficile most often occurs in older adults or people who are in hospital or have recently had antibiotics.
- Symptoms can range from mild diarrhoea to a life-threatening inflammation of your bowel.
- If it's very mild, you may get better on your own. Otherwise, treatment with specific antibiotics is generally needed.
- Symptoms come back in about 1 in 5 cases and treatment may need to be repeated.
- C. diff is contagious. Washing your hands with soap and water, especially after using the toilet and before eating or drinking, is especially important in reducing and preventing the spread.

Healthy people don't usually get C. diff infections. You're more likely to get this infection after you've taken antibiotics, if you're over 65 years of age or are in a hospital or long-term care facility (nursing home).
Factors that increase your risk of C. diff infection
- Taking antibiotics: Taking antibiotics can increase your risk of C. diff infection, especially if you have been taking antibiotics that work against several types of bacteria (broad-spectrum antibiotics) or several different antibiotics at the same time, or taking antibiotics long-term. You're also at greater risk of getting this disease if you have low immunity.
- Being in hospital or in a nursing home: This increases the risk of C. diff infection. Many cases start in the community, especially in nursing homes. Generally the longer your stay in hospital and the older you are, the greater your risk of developing C. diff infection.
- Older adults: C. diff infection is more common in older people. More than 8 in 10 cases occur in people over the age of 65. This is partly because older people are more commonly in hospital. Also, older people seem to be more prone to this infection – possibly due to weakened immune systems or having other medical problems that put them at greater risk. Infection is less likely in children.
- Previous C. diff infection: If you have had C. diff infection once, you are at higher risk of having the infection again in the future. Having had the C. diff infection can make your bowel more sensitive to antibiotics.
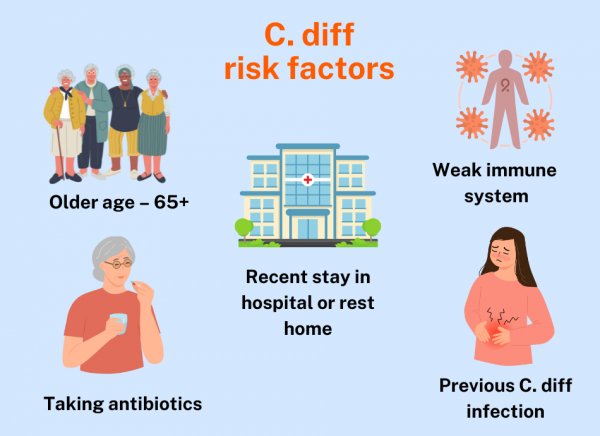
Image credit: Healthify He Puna Waiora
C. diff can spread easily to other people because the bacteria are passed out of your body in your diarrhoea. Once out of your body, the bacteria turn into spores (bacteria with a protective coating). These are designed to survive outside the human body.
They can survive for a very long time on surfaces (eg, toilets, commodes and bed frames), objects and clothing. If these aren't thoroughly cleaned, they can infect someone else.
C. diff can also spread on your hands if you have direct contact with someone who is infected or if you touch contaminated surfaces. If you then touch your mouth, you may swallow the spores.
The main symptom is having at least 3 watery poos daily for 2 days or more. Other symptoms include fever, loss of appetite, nausea and stomach pain or cramp. There are different strains of C. diff and some can cause a more serious illness than others.
In most cases, the symptoms start within a few days of starting the antibiotic. However, in some cases, symptoms develop up to 10 weeks after finishing a course of an antibiotic.
Diagnosis
If your healthcare provider suspects you have a C. diff infection, a faeces (poo) sample can be tested in the laboratory to confirm the diagnosis. The test looks for the toxin (poison) that's produced by C. diff in the poo sample. Blood tests, an X-ray of your abdomen (tummy) or a CT scan may be suggested if you have more severe infection.
Treatment
The decision about whether to treat C. diff infection and the type of treatment depends on the severity of the illness. No treatment is needed if you have no symptoms but you're known to carry the bacteria in your gut. Sometimes your healthcare provider may just stop (if possible) the antibiotics you may be taking or other medicines, eg, proton pump inhibitors (PPIs).
If you have symptoms you will usually be treated with a specific antibiotic (usually metronidazole). This antibiotic targets the C. diff bacteria and allows the good bacteria in your gut time to recover. It's important you complete the whole course of antibiotics or the infection may come back.
Occasionally, if the infection is very severe, surgery to remove the infected bowel is needed. If it keeps coming back or doesn't respond to usual treatment, a faecal (poo) transplant is sometimes helpful.
Good hand hygiene is especially important to reduce the risk of spreading C. diff infection. This includes washing your hands with soap and water, especially after using the toilet and before eating or drinking.
Washing your hands with soap and water is much better at preventing the spread of diarrhoea than using alcohol-based hand rubs. Alcohol-based cleaners don't kill the C. diff spores.
Once the diarrhoea stops, the risks of spreading C. diff infection are much lower. Read more about hand washing.
If you are in hospital
If you're in hospital, you'll be placed in isolation to reduce the risk of spreading C. diff infection to other patients. This means you'll be in your own room and have your own toilet. Hospital staff caring for you may wear gloves and gowns or aprons to prevent them carrying the bacteria to other patients. If you're in isolation, don't visit patients in other parts of the ward or in other wards. You may also be asked not to go into public areas.
Healthy visitors, including pregnant women, can carry on visiting you in hospital as they aren't at an increased risk of infection. But your visitors must wash their hands with soap and water when they leave your room. It's unlikely that the bacteria will be transmitted if everyone keeps up good hand hygiene. Your family can take your laundry home and wash it as usual.
C. diff infection won't stop you going home from hospital. You'll be discharged as soon as your general condition allows. Complete your course of antibiotics as prescribed even if you're feeling better.
When you get home
At home, maintain good personal hygiene and household cleaning. Good hand washing is very important. Wash your hands well after using the toilet and before eating. Keep the toilet clean. Clean surfaces in bathrooms, kitchens and other areas regularly with household detergents and disinfectants. If your symptoms come back, talk to your healthcare provider as you may need further treatment.
What is C. diff?(external link) Center for Disease Control, US
Brochures
C. diff factsheet(external link) CDC, US
The progression of a C. diff infection(external link) CDC, US
References
- Clostridioides difficile (C. diff)(external link) Center for Disease Control, US
- Clostridium difficile colitis(external link) Antibiotic Guide, BPAC, NZ, 2017
Trubiano JA, Cheng AC, Korman TM et al. Australasian Society of Infectious Diseases updated guidelines f(external link)or the management of Clostridium difficile infection in adults and children in Australia and New Zealand(external link) Internal Med J 2016;46(4):479-493
Primary care antibiotics guide(external link) BPAC, NZ, 2024
Clostridium difficile infection – NZ perspective(external link) – Dr Sally Roberts, Infectious Diseases Physician and Clinical Microbiologist, Auckland DHB and HQSC, NZ, 2019
Clostridium difficile infection (CDI) – issues around surveillance and notifiability(external link) – Dr John Holmes, Public Health Medicine Specialist, ESR and University of Otago, NZ, 2019
Brochures

CDC, US
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed: