You can now add Healthify as a preferred source on Google. Click here to see us when you search Google.
Chronic pancreatitis | Mate repe huka kōpauku
Key points about chronic pancreatitis
- Your pancreas is part of your digestive system.
- It releases chemicals called enzymes to help with the breakdown of food and insulin to help regulate blood glucose levels.
- Chronic pancreatitis (mate repe huka kōpauku) occurs when your pancreas becomes permanently damaged from inflammation.
- This is different to acute pancreatitis, where the pancreas becomes inflamed for a short period of time.
- Chronic pancreatitis is usually caused by heavy drinking but it has also been linked to smoking.

Your pancreas is a small organ located behind your stomach and below your ribcage. It's a part of your digestive system. It releases enzymes, or digestive juices, into your small intestine to further break down food after it has left your stomach. It also secretes the hormone insulin into your bloodstream to regulate your glucose levels.
The image below shoes the location of your pancreas.
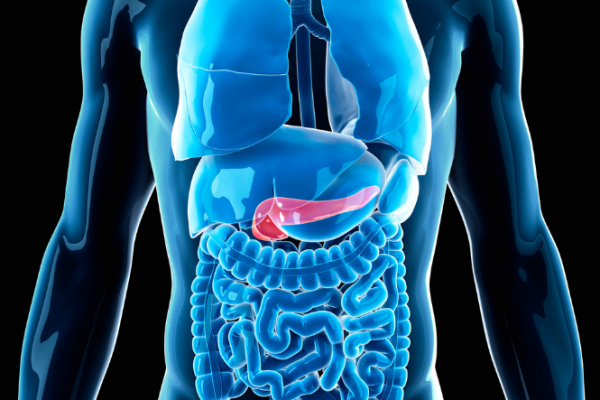
Image credit: Canva
Chronic pancreatitis happens when your pancreas becomes permanently damaged from inflammation. This inflammation is usually caused by heavy drinking, although smoking has also been found to be linked to chronic pancreatitis. The inflammation causes scarring and damage to parts of the pancreas, which affect its ability to produce digestive enzymes and insulin.
Chronic pancreatitis can affect people of any age, but is most common in men between 45 and 54 years of age.
Having chronic pancreatitis increases your risks of getting pancreatic cancer. Treatment manages symptoms but it can't repair damage. This means chronic pancreatitis can affect your life quite a lot, and getting support is important.
Video: Chronic pancreatitis signs and symptoms
This video may take a few moments to load.
(The National Pancreas Foundation, US, 2013)
Long-term alcohol misuse is responsible for around 7 out of 10 cases of chronic pancreatitis.
Less common causes:
- Smoking.
- Some rare genetic conditions, (eg, cystic fibrosis) or auto-immune conditions (eg, Sjögren's disease) and a liver disease called primary biliary cirrhosis, can also increase your chance of getting chronic pancreatitis.
The cause can't be identified in up to 3 out of 10 people.
The most common symptom of chronic pancreatitis is repeated episodes of pain, just below your ribs, which may extend into your back. It may be mild at first but can become quite severe. Eating can make the pain worse. However, 1 in 5 people have no pain.
You may also feel nausea (sick), have problems with your digestion (because the pancreas isn’t producing enough enzymes) or develop diabetes (because your pancreas isn’t producing enough insulin. Over time, you may have greasy, foul-smelling stools.
Diagnosis
Because it can be difficult to diagnose chronic pancreatitis, your healthcare provider may ask you to have a few tests, including blood tests, a stool sample, X-ray, CT scan or MRI.
Treatment
The key treatment is to stop drinking alcohol for the rest of your life. You will probably also be prescribed painkillers and other medication if needed to help with your enzyme or insulin levels. You will also be advised to stop smoking and avoid fatty foods.
There's no treatment to repair the damage that has already happened to your pancreas. Surgery is sometimes needed to treat severe chronic pain that doesn't respond to painkillers.
Living with chronic pain can affect your mental health. Talk to your healthcare provider if you're finding it difficult to cope, and they can recommend a counsellor or therapist to help you.
Medicines
Depending on the cause of your pancreatitis and your symptoms, you may be prescribed medicines to help you feel better.
- You may be prescribed medicines to relieve pain, such as paracetamol and ibuprofen for mild pain, and stronger painkillers such as morphine or tramadol for severe pain.
- To help improve your digestion, you may be given tablets containing the enzymes normally made by your pancreas.
- If your pancreatitis is caused by problems with your immune system, you may be prescribed corticosteroids to reduce inflammation of the pancreas.
The best thing you can do for yourself is to stop drinking. Tell your doctor if you need support to do this. You will also help yourself if you:
- quit smoking
- avoid fatty foods
- eat several small meals per day rather than 3 large meals
- take any medicine as prescribed
- get help if you're finding it difficult to cope.
Apps reviewed by Healthify
You may find it useful to look at some Alcohol use apps, Quit smoking apps and Nutrition, exercise and weight management apps.
There are online support groups for people with chronic pancreatitis, eg, Facebook support group for chronic and acute pancreatitis(external link)
You can also find a counsellor(external link) to talk to about living with this condition.
The best way to prevent chronic pancreatitis is to either avoid alcohol, or if you do drink it, stick to the recommended daily and weekly limits for drinking alcohol. Quitting smoking and eating a healthy diet may also reduce your risk of getting chronic pancreatitis.
Chronic pancreatitis(external link) NHS Choices, UK
Chronic pancreatitis(external link) Patient Info, UK
Alcohol & you – facts & effects [PDF, 5.3 MB] Health Promotion Agency, NZ, 2020
Apps
Alcohol use apps
Quit smoking apps
Nutrition, exercise and weight management apps
References
- Chronic pancreatitis(external link) Patient Info, Doctor, UK, 2022
- Chronic pancreatitis(external link) NHS Choices, UK, 2022
- Cancer of the pancreas(external link) NHS Choices, UK, 2023
- Alsamarrai A, Das SLM, Windsor JA, et al. Factors that affect risk for pancreatic disease in the general population – a systematic review and meta-analysis of prospective cohort studies(external link) Clin Gastroenterol Hepatol. 2014;12(10):1635–164.
Diagnosis of chronic pancreatitis
Chronic pancreatitis can be hard to diagnose, with examination often largely unremarkable apart from tenderness in the abdomen. Consider chronic pancreatitis if patient presents with episodes of exacerbation with intervening remission or continuous abdominal pain, classically, epigastric pain radiating into the back. Usually the pain is very severe, which often requires opiates in the acute setting. In some cases, though, pain may not be the major feature. Other symptoms include:
- nausea and vomiting
- decreased appetite
- exocrine dysfunction. Malabsorption with weight loss, diarrhoea, steatorrhoea (pale, loose, offensive stools which are difficult to flush) and protein deficiency
- endocrine dysfunction. Diabetes mellitus and its associated morbidity and mortality.
Differential diagnosis of abdominal pain:
- acute cholecystitis
- peptic ulcer disease
- acute hepatitis
- abdominal aortic aneurysm
- pyelonephritis
- acute pancreatitis
- non-abdominal causes, eg, myocardial infarction and pneumonia.
Differential diagnosis of pancreatic calcification on abdominal imaging:
- severe protein malnutrition.
- hereditary pancreatitis.
See more at www.patient.info/doctor/chronic-pancreatitis-pro(external link)
BPAC. Substance misuse and addiction in Māori. Best Practice Journal, 2010 June. www.bpac.org.nz/BPJ/2010/June/addiction.aspx(external link)
D'Haese JG, Ceyhan GO, Demir IE, Tieftrunk E, Friess H. Treatment options in painful chronic pancreatitis: a systematic review. HPB 2014; 16(6): 512-521. www.ncbi.nlm.nih.gov/pubmedhealth/PMH0068367(external link)
Turner R. Chronic pancreatitis – negotiating the complexities of diagnosis and management(external link) Aust Fam Phys 2015;44(10):718-722
Continuing professional development
Chronic pancreatitis(external link) Goodfellow Podcast, NZ, 2019
Professor John Windsor talks about chronic pancreatitis. John is a trained general surgeon who has had further fellowship training in hepato-biliary and pancreatic, gastro-oesophageal and laparoscopic surgery. He works at Auckland City Hospital and the University of Auckland. Privately he works at Mercy Hospital in Auckland and specialises in pancreatic, biliary, gastric and oesophageal surgery.
Apps
Alcohol use apps
Quit smoking apps
Nutrition, exercise and weight management apps
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Art Nahill, Consultant General Physician and Clinical Educator
Last reviewed:





