If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Haemophilia
Key points about haemophilia
- Haemophilia is a rare bleeding disorder affecting your blood's ability to clot and making you bleed for longer than usual.
- The most common bleeding disorders are haemophilia and von Willebrand disease.
- Haemophilia is usually inherited and most people who have it are male, but women can have it.
- The main symptom is bleeding that doesn’t stop, but you may also notice your skin bruises easily.
- Clotting factor medicines are used to replace the missing clotting factors to control bleeding.
- Haemophilia is a lifelong condition but it can be managed so that you can live a normal life.

Haemophilia is a treatable lifelong bleeding disorder that makes you bleed for longer than usual.
When most people cut themselves, proteins called clotting factors combine with blood cells called platelets to make their blood sticky. This makes the bleeding stop eventually. However, if you have haemophilia, you have lower than normal levels of clotting factor in your blood. This means your blood doesn’t clot properly and you bleed for longer than usual.
There are 2 types of haemophilia
- Haemophilia A – this is the most common type and is caused by having low levels of clotting factor VIII (factor 8). Recent studies indicate that about 87% of people with haemophilia have haemophilia A.
- Haemophilia B – this is the second most common type and is caused by having low levels of factor IX (factor 9). It's sometimes known as Christmas disease.
It's important to note that these are different diseases. Even though they are inherited in the same way and have the same symptoms, they're treated differently.
Symptoms of haemophilia usually begin in childhood, but sometimes may not be noticed until later. It’s important to know what type of haemophilia you, or your child has, as treatment will depend upon this. A medicine will be given to replace the missing clotting factor in your blood to control bleeding.
Haemophilia is caused by a mutation (fault) in 1 of your genes. This happens in 2 ways:
- 70% of the time it’s an inherited condition, which means it’s passed down from parent to child
- 30% of the time its a spontaneous mutation (just happens) and there's no family history.
Very rarely, it can appear unexpectedly later in life – this is called acquired haemophilia. This type is caused by a problem with your immune system, involving an antibody that attacks a clotting factor. Acquired haemophilia is treated differently to the haemophilia you're born with.
If you inherit the abnormal gene that causes haemophilia, you’ll have lower than normal levels of a clotting factor. It's considered a rare condition that mainly affects males – 1 in 10,000 people born in Aotearoa New Zealand has haemophilia.
Interestingly there are more female carriers than affected males. A carrier is someone who has the gene and can pass it on to their offspring. Female carriers can be affected and have low levels of clotting factor (symptomatic) or not affected (have no symptoms or be asymptomatic).
Read more about the inheritance of haemophilia(external link).
There are other conditions, such as von Willebrand disease, that can cause symptoms that are similar to haemophilia.
The symptoms of haemophilia can be mild to severe depending on the level of clotting factor deficiency you have. Sometimes bleeding can happen without injury (spontaneous) or can result from trauma, such as a cut or a dental procedure. There are many signs of haemophilia depending on the severity, the site of your bleeding and your age.
The main symptom is bleeding that doesn't stop (prolonged bleeding). For many people with haemophilia, the bleeding won’t stop without an injection of the appropriate clotting factor medicine. Bleeding can be external or internal.
External bleeding is bleeding on the outside of your body, where it can be seen. You may notice:
- nosebleeds that take a long time to stop
- bleeding from wounds that lasts a long time
- bleeding gums.
Internal bleeding is bleeding on the inside of your body (eg, in your joints, muscles, and internal organs) where it's not seen and is harder to identify. You may notice:
- easy and often large bruising
- unexplained pain or swelling
- fatigue or weakness
- being suddenly unable to move a limb
- blood in urine or stool
- unusual behaviour, being irritable, having a headache or vomiting (being sick) after a head knock.
Undiagnosed haemophilia
If the haemophilia is unknown and undiagnosed, bleeding problems usually occur after an injury, after dental work or medical procedures. However, people with mild haemophilia may have no abnormal bleeding until they have surgery.
Babies
At birth:
- bleeding is sometimes seen around the umbilical cord
- bruising can happen at the heel pick site, or
- a failed attempt to put in an intravenous (IV) cannula may result in a muscle bleed
- a head bleed if the haemophilia is severe.
During their first year, the first signs of haemophilia are usually heavy bleeding from the mouth from bites to their gums and tongue, or severe bruising.
If your child is very young, you may notice they have difficulty using or straightening a joint. The joint might look swollen and feel hotter than the same joint on the other side of their body. Your child may limp or avoid putting their heel on the floor when walking or standing.
Importance of recognising symptoms
Recognising the symptoms will assist with a good outcome. Symptoms will vary depending upon the sites involved. Always assess the injured site quickly and keep checking. Bleeding into certain spaces, such as your head, throat, spine, chest, abdomen and limb compartment (groups of muscles, nerves, and blood vessels in your arms and legs) is serious and needs quick medical treatment.
If you suspect you or your child has haemophilia, based on the symptoms listed above, see a healthcare provider.
You’ll be examined and asked about whether you have a family history of bleeding disorders. You’ll also be asked to have a blood test which can diagnose haemophilia and find out how severe it is based on how low your clotting factor levels are.
If there's no family history of haemophilia, it's usually diagnosed when a child begins to walk or crawl. Mild haemophilia may only be discovered at a later age, usually after an injury or a dental or surgical procedure.
Everyone with haemophilia should be registered with a Regional Haemophilia Centre and reviewed by a haematologist (a doctor who specialises in blood disorders).
Haemophilia can be treated safely and effectively with the use of clotting factor medicines to replace the missing clotting factor in your blood (either factor VIII or factor IX) and help your blood to clot normally. The aim of treatment is to reduce the risk of long-lasting complications, heavy bleeding and damage to joints.
Most of the clotting factor replacements used today are called recombinants which are man-made, non-viral and work well. These products are given as concentrates (called factor concentrates or factor replacements), which are infused, or injected, into your blood. Because they’re very concentrated, a small amount can control serious bleeding – even during surgery.
Products made from plasma in human blood are occasionally used in certain settings or as a patient preference. They're more commonly used to treat other, rarer bleeding disorders.
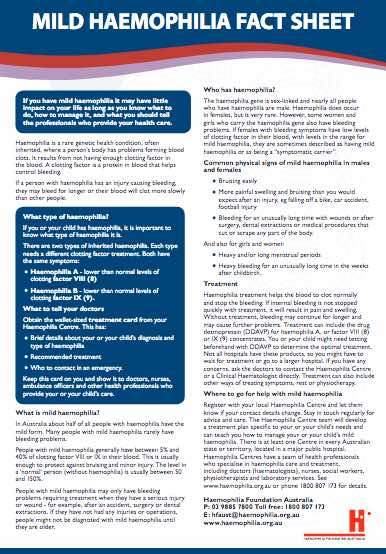
Approaches to treatment
There are 2 main approaches to treatment, depending on how severe your haemophilia is.
- Preventative (prophylaxis) therapy – where you receive regular injections of clotting factor medicine to help prevent episodes of bleeding, protecting your joints and muscles.
- On-demand therapy – where you’re given an injection of clotting factor when you have a bleeding episode. This done even for mild or moderate haemophilia
Preventative therapy gives children the best chance to reach adulthood without damage to their joints.
Treatment of a bleed
Early treatment of any bleed is essential to minimise any long-term damage and limit how much it disrupts your daily life.
If you’re treating a bleed at home or outside of the hospital, you should:
- take your clotting factor medicine as soon as possible
- start to follow the PRICE regimen
- let your haemophilia centre know
- arrange for an appointment to see your physiotherapist for assessment and advice – Physiotherapy following a bleed is important to help with recovery from internal bleeding that may have damaged your joints.
PRICE regimen

Image credit: Healthify He Puna Waiora
- Protection – Protect your joint by not putting weight on it for at least the first 48 hours and possibly longer if it’s a severe bleed. Use crutches or other supports.
- Rest – Completely rest the affected area to allow the swelling to ease and prevent further bleeding, but remember that too much rest can also be damaging, so start to move the joint gently within 1 to 2 days of treatment.
- Ice – Applying ice helps to reduce swelling, prevent further bleeding and ease pain. Don’t place ice directly on your skin as it can burn. Instead use a gel cold pack or make a cold pack from a bag of frozen peas or crushed ice wrapped in a cloth. Apply this to the affected area for around 10 to 15 minutes every 2 hours – don’t apply it for more than 20 minutes at a time.
- Compression – Apply pressure and a bandage to the affected area to reduce swelling and pain. Your physiotherapist can provide you with an elasticated bandage and will make sure it fits properly. A bandage that fits too tightly can cause more damage. Try not to allow wrinkles in the bandage and remove it at night.
- Elevation – Raise the injured area above the level of your heart. This increases blood flow away from the injured area and reduces swelling and pain. When you elevate your leg, remove your compression stocking to allow for normal blood circulation. Elevate the area for about 20 minutes at a time.
Managing pain
You’ll also need treatment to manage pain as swelling caused by bleeding, especially in your joints, can be extremely painful. The more swollen an injury becomes, the more pain you’ll feel. You need to avoid aspirin and most non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen as they stop platelets from working and reduce blood clotting. Talk to your healthcare provider or pharmacist about possible side effects before taking any pain medicines.
Yes, girls can have haemophilia! It’s rare but it happens. Many women are unaware and will struggle with bleeding that affects their quality of life. They are often diagnosed later and will have different healthcare needs to men.
The treatment for girls and women with reduced factor VIII levels is the same as the boys, with the exception of hormone therapy. Managing heavy periods (menorrhagia), pregnancy, childbirth and menopause is challenging if you have haemophilia and can lead to low iron levels or anaemia. Getting checked and being given the right care is vital.
Talk to your local haemophilia centre if:
- you or your partner have haemophilia
- you have a family history of haemophilia
- you're planning to have a baby
- you're already pregnant.
This can be a complex time and it's advisable to plan your pregnancy in advance. The haemophilia team involved will be happy to help, so you feel supported and informed. These centres can refer you to genetic counselling to understand the available options. They work closely with obstetrics teams to manage the bleeding risks at the time of delivery – for both mum and child.
Bleeding
Repeated bleeding in and around your joints causes damage and if it becomes severe, you may need joint replacement in the future. This is similar to the damage and pain caused by arthritis, but if you have haemophilia you’re likely to experience it at an earlier age.
Inhibitor development
Some people with haemophilia develop antibodies, called inhibitors, to the clotting factor medicines. This means the medicines won’t be effective anymore and bleeding can’t be controlled quickly. For these people, there’s a risk of permanent damage from bleeding into joints or death from serious internal bleeding.
Infection
In the past, there’s also been the risk of infection from blood-borne viruses in some treatments. Things have improved and in Aotearoa New Zealand, all donated blood is strictly screened for known blood-borne viruses and the risk is very low. The recombinant clotting factors (man-made) medicines are the main treatments used and they are very safe and effective.
Emotional impact
Having haemophilia isn't easy. The need to be constantly careful, avoid certain activities and watch for bleeding can affect how you live your life and how you feel about yourself. The need for quick treatment (by injection/infusion), management of pain and having to change plans with little or no warning can also be difficult. It's important to get the support you need. There are people to talk to if you are finding life with haemophilia challenging or you're caring for a child with haemophilia. You can ask to see a counsellor or find out who to contact in the support section below.
With proper treatment, life expectancy for people with haemophilia is almost the same as those without haemophilia, and most people can enjoy a good quality of life.
Gene therapy can provide a possible cure for haemophilia and is registered for use in some countries, but it’s not yet available in Aotearoa New Zealand.
If you or your child have haemophilia, good self-care includes:
- knowing the type (haemophilia A or B) and severity (mild, moderate or severe) of haemophilia you or child has so that you can tell any healthcare provider who treats you
- avoiding contact sports, unless you’ve been told it’s safe to take part
- regular exercise to keep joints healthy
- being careful taking other medicines – some, such as aspirin and ibuprofen, can affect your blood's ability to clot
- looking after your teeth well and having regular trips to the dentist so you don’t develop gum disease (which can cause bleeding)
- talking to your haemophilia care providers before having any surgery or dental treatment
- wearing a MedicAlert bracelet, or similar form of identification, in case you have severe bleeding or trauma.
If you have mild haemophilia, follow the PRICE regimen if you have a mild injury.
Haemophilia New Zealand(external link) supports and represents people with haemophilia and other related bleeding disorders in Aotearoa New Zealand. They run a number of programmes and services for people with bleeding disorders and their families. They have Haemophilia Outreach Workers(external link) providing support in different regions of the country. Haemophilia New Zealand also run camps and workshops(external link) for people who are affected and their whānau.
There are 6 Haemophilia Centres across Aotearoa New Zealand who all provide a comprehensive service for people with haemophilia, and other bleeding conditions, and their families. Services include annual clinic reviews, bleeding advice, treatment and genetic counselling.
The following links provide further information about haemophilia. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
How do I recognise a bleed and what should I do?(external link) Auckland Haemophilia Centre, Health New Zealand | Te Whatu Ora, NZ
Haemophilia – a guide for parents of a newly diagnosed child(external link) Haemophilia Foundation, Australia
Haemophilia(external link) Haemophilia New Zealand
Brochures
Haemophilia(external link) Haemophilia Foundation, Australia
Mild haemophilia fact sheet(external link) Haemophilia Foundation, Australia
References
- Haemophilia(external link) NHS, UK, 2025
- Haemophilia(external link) Haemophilia New Zealand, NZ
- How do I recognise a bleed and what should I do?(external link) Auckland Haemophilia Centre, Health New Zealand | Te Whatu Ora, NZ
- New Zealand National Guidelines for the Management of Haemophilia 2022(external link) National Haemophilia Treaters Group, Te Whatu Ora | Health New Zealand, NZ, 2022
- Abnormal bleeding or bruising(external link) Auckland HealthPathways, NZ, updated 2024
- Haemophilia(external link) Haemophilia Foundation, Australia, 2024
- Haemophilia A – Factor VIII deficiency(external link) Patient Info Professional, UK, 2024
- Haemophilia(external link) Patient Info, UK, 2023
- History(external link) National Bleeding Disorders Foundation, US
- Report on the 2020 global survey(external link) World Federation of Hemophilia, 2021
New Zealand national guidelines for the management of haemophilia 2022(external link) National Haemophilia Treaters Group, Te Whatu Ora | Health New Zealand, NZ, 2022
Haemophilia A – Factor VIII deficiency(external link) Patient Info Professional, UK, 2024
Rayment R, Chalmers E, Forsyth K, et al. Guidelines on the use of prophylactic factor replacement for children and adults with Haemophilia A and B(external link) Br J Haematol. 2020 Sep;190(5):684–695
Srivastava A, Santagostino E, Dougall A, et al. WFH Guidelines for the Management of Hemophilia, 3rd edition(external link) Haemophilia 2020 Aug;26 Suppl 6:1–158
Pavord S, Rayment R, Madan B, et al. on behalf of the Royal College of Obstetricians and Gynaecologists Management of inherited bleeding disorders in pregnancy. Green-top Guideline No. 71(external link) BJOG 2017; 124:e193–e263
What is haemophilia?
Haemophilia is a rare bleeding disorder that makes you bleed for longer than usual because your blood doesn’t clot properly. It's due to having low levels of a clotting factor in your blood and is usually an inherited condition.
How common is haemophilia?
It's a rare condition, about 1 in 10,000 people in Aotearoa New Zealand has haemophilia. It's more common in males than females. Based on a global survey in 2020, the World Federation of Hemophilia suggested there are an estimated 815,100 people around the world with haemophilia.
Why is haemophilia called royal disease?
Hemophilia is sometimes called 'the royal disease' because it affected the royal families of England, Germany, Russia and Spain in the 19th and 20th centuries. Queen Victoria (great-great-great grandmother to King Charles) is thought to have been a carrier of haemophilia B and passed it on to some of her children. Haemophilia was carried through various royal family members for another 3 generations before disappearing.
Brochures

Haemophilia Foundation, Australia, 2013
Haemophilia Foundation, Australia, 2013
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Vanessa Minor, Haemophilia Nurse Specialist, Auckland
Last reviewed:





