If you're a frequent visitor to Healthify, why not share our site with a friend? Don't forget you can also browse Healthify without using your phone data.
Diabetes-related foot ulcer
Also called diabetic foot
Key points about diabetes-related foot ulcers
- People with diabetes have an increased chance of developing foot problems such as foot ulcers. This is commonly known as 'diabetic foot'.
- A foot ulcer is a slow-healing open sore that develops on your foot – an infected diabetic ulcer is a serious problem.
- Ask your doctor to examine your feet regularly for any sign of nerve damage or poor circulation.
- Ask your doctor to refer you to a podiatrist if you have been told that you are at higher risk of diabetes-related foot disease and to a Specialist Diabetes Foot Clinic if you develop a foot problem such as a foot ulcer.
- Foot problems can be avoided if you take care of your feet and act quickly if you have a problem.

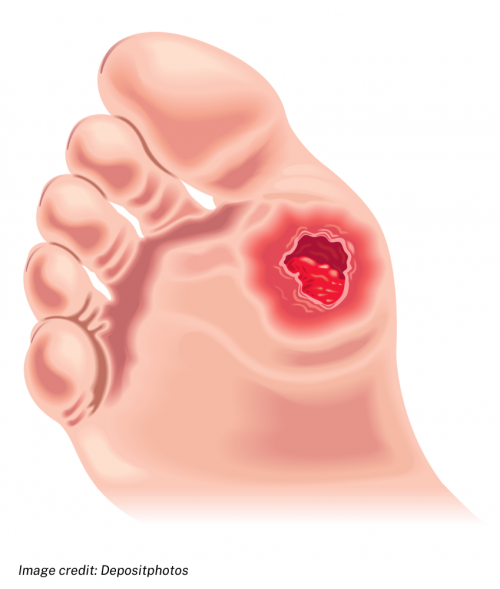
A foot ulcer is an open sore or wound on your foot that is slow to heal because of your diabetes, and sometimes there are circulation problems too.
If it gets infected it can be very serious.
If you have diabetes you have a greater chance of developing foot ulcers because you’re more likely than other people to not notice if you damage the skin on your feet. This is because diabetes can cause nerve damage, so you don't notice if your foot is injured or sore. Diabetes also causes sores to heal slowly and causes blood vessel damage so your skin can't heal easily.
- About 1 in 4 people with diabetes (25%) will develop a foot ulcer sometime during their life, and about 50% of those ulcers will become infected.
- 1 in 5 (20%) people with a severe foot infection may end up with an amputation. In fact amputations are 15 times more common in people with diabetes than in those without.
You are at low risk for diabetes-related foot problems if:
- you have feeling in your feet
- your feet have a good blood supply.
You are at moderate risk for developing diabetes-related foot problems if you have 1 of these risk factors:
- you have lost some feeling in your feet (loss of protective sensation)
- you have reduced circulation in your feet (peripheral arterial disease)
- you have corns or calluses (hard skin) on your feet
- you have foot deformities (eg, bunions, claw toes, hammer toes)
- you have end stage kidney disease.
You are at high risk for diabetes-related foot problems if:
- you have more than 1 of the foot problems in the moderate risk category
- you have had ulcers before
- you have had an amputation
- You have a foot deformity called a Charcot Foot.
Foot ulcers are open sores or wounds that occur most often on the ball of your foot or on the bottom of your big toe. They may also develop on the side of your foot, usually because of poorly fitting shoes. The ulcers are usually painless. Not all diabetes-related foot ulcers become infected but if you have diabetes you are at high risk of developing infection of the ulcer and the surrounding skin (cellulitis). Infected diabetes-related ulcers are a serious problem and need urgent attention.
Depending on the severity of the wound and the presence of infection, diabetes-related foot ulcers can be classified in 4 ways:
- Uninfected – the wound doesn't have signs of infection.
- Mild infection – the area around the wound may be warm to the touch, red, slightly swollen, painful or tender, and the wound/ulcer may ooze pus.
- Moderate infection – foot infection that involves the deeper layers of your skin, into the muscle, tendons, bone or joints.
- Severe infection – foot infection that causes sepsis (which is a life-threatening complication of infection). The symptoms of sepsis are high body temperature (fever), fast heartbeat, and heavy or quick breathing.
If you have diabetes and notice a sore or blister on your foot, contact your healthcare provider immediately. If ulcers aren't treated it can result in infection, which can cause loss of a limb. This can be avoided if you take care of your feet and act quickly if you have a problem.
Treatment of the foot ulcer depends on the severity of the wound.
Severity |
Treatment |
|
All |
|
|
Not infected |
|
|
Mild infection |
|
|
Moderate infection |
|
|
Severe infection |
|
Lifestyle factors that improve wound healing
In addition to managing the wound, attention to other lifestyle factors can also contribute to improved wound healing.
- Maintain good blood glucose management.
- Treat high blood pressure and high cholesterol.
- Stop smoking.
- Eat a healthy diet.
- Keep active – if you have a foot ulcer, your podiatrist will advise when this is appropriate.
- Manage your weight (if needed).
Apps reviewed by Healthify
You may find it useful to look at some Diabetes apps.
You can lower your risk of developing diabetes-related foot problems by:
- keeping your blood glucose in your target range
- managing your blood pressure and cholesterol levels
- looking after your feet and checking them daily (ask someone to help if you can’t reach them or see well enough to check them)
- eating a healthy diet
- staying active and exercising
- not smoking.
Learn more about diabetes and foot care.
Video: Preventing diabetic complications with foot and skin care
When you have diabetes, it's important to take extra care of your feet to prevent ulcers and other complications.
If the foot ulcer doesn't heal, becomes worse or badly infected, or if the infection spreads to nearby bones or joints, this can lead to gangrene. The only solution then may be to surgically remove (amputate) the affected part.
There are many groups and people keen to share their knowledge and tips for living well with diabetes. Diabetes New Zealand(external link) has branches around the country with a wide range of services, resources, groups and shops.
Regional diabetes support
- Diabetes New Zealand Auckland branch and website(external link)
- Diabetes Help Tauranga(external link) Phone 07 571 3422 for their diabetes helpline. Also offers network groups, drop-in services, counselling services, diabetes courses, registered diabetes nurse specialist.
- Diabetes Trust (Palmerston North)(external link) Phone 06 357 5992. Offers education courses, youth and family support, personal stories and more.
- Diabetes Wellington(external link)
- Diabetes Christchurch (external link)
- Diabetes New Zealand – all regions(external link)
The following links provide further information on diabetic foot ulcer. Be aware that websites from other countries may contain information that differs from New Zealand recommendations.
Diabetic foot ulcers(external link) DermNet NZ
Diabetes, foot care and foot ulcers(external link) Patient Info, UK
The right steps to healthy feet(external link) Diabetes New Zealand
Feet(external link) Diabetes New Zealand
Diabetes and foot problems(external link) Diabetes UK
Type 2 diabetes – health problems(external link) NHS, UK
Resources
Diabetes feet care checklist(external link) Diabetes Feet Australia
Know your risk diabetes(external link) Diabetes New Zealand
Diabetes and how to care for your feet(external link) Diabetes New Zealand
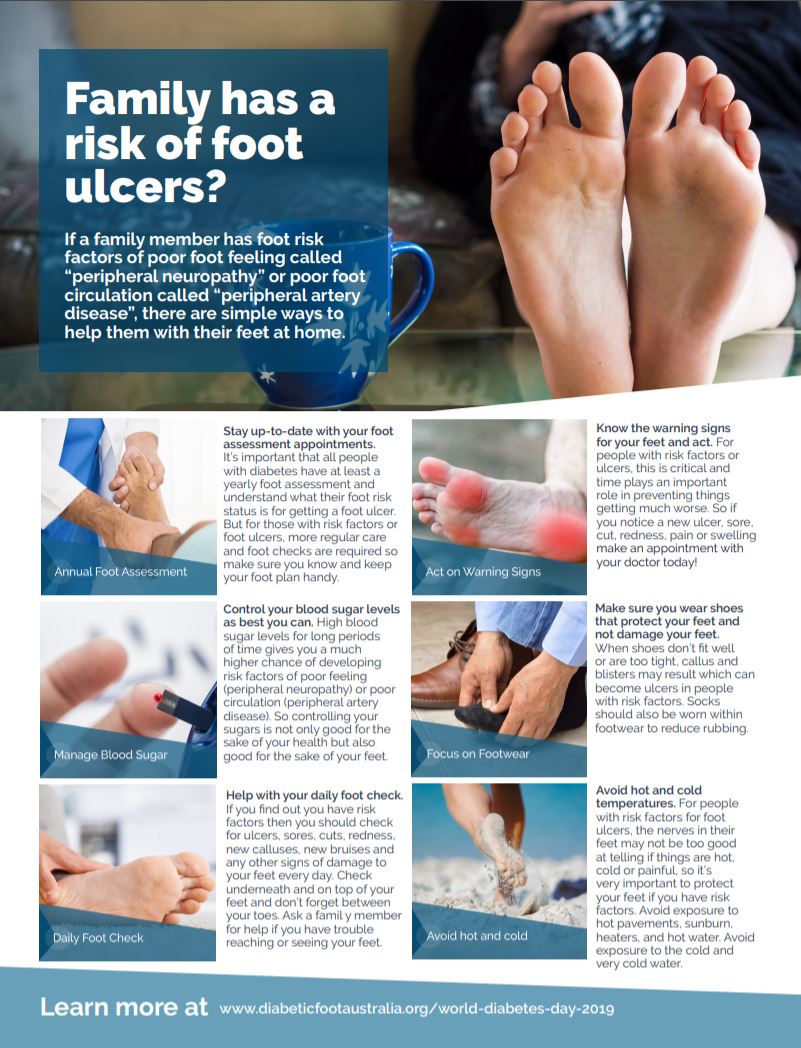
Family has a risk of foot ulcers?(external link) Diabetic Foot Australia
Apps
References
- Diabetic foot problems – prevention and management(external link) NICE Guideline, UK, updated 2019
- IWGDF/IDSA guidelines on the diagnosis and treatment of diabetes-related foot infections(external link) (IWGDF/IDSA 2023)
- International best practice guidelines – wound management in diabetic foot ulcers(external link) Wounds International, 2013
- Diabetes and how to care for your feet(external link) Diabetes New Zealand, 2023
- The right steps to healthy feet(external link) Diabetes New Zealand
- Feet(external link) Diabetes NZ
- Diabetes and foot problems(external link) Diabetes UK
- Type 2 diabetes – health problems(external link) NHS, UK, 2023
Clinical pathways and assessment forms for diabetic foot
Best Practice diabetes toolbox(external link) BPAC, NZ, 2021
Diabetes (the high risk foot)(external link) NZ Society for Study of Diabetes (NZSSD), Podiatry Special Interest Group (PodSIG), NZ, 2017
Primary care/district nursing diabetic foot assessment form(external link) Diabetic Foot Ulcer Group, NZ, 2011
Secondary care diabetic foot ulcer assessment Form(external link) Diabetic Foot Ulcer Group, NZ, 2011
Diabetes feet health passport(external link) Diabetes Feet Australia
IWGDF guideline on the prevention of foot ulcers in persons with diabetes(external link) International Working Group on the Diabetic Foot Guidelines, 2019
IWGDF guideline on offloading foot ulcers in persons with diabetes(external link) International Working Group on the Diabetic Foot Guidelines, 2019
See our page Diabetes for healthcare providers
Continuing professional development
Diabetic foot disease(external link) Goodfellow eLearning, NZ, 2019
Brochures
Diabetic Foot Australia, 2019
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Michele Garrett, Professional Leader Podiatry | Te Toka Tumai, Waitematā & Metro Auckland Foot Protection Services
Last reviewed:






