Telehealth is a broad term that can also include activities not directly relating to patients, such as providing education or training sessions and video conferencing for meetings.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Telehealth for healthcare providers
Key points about telehealth
- Telehealth is defined by the National Health IT Board as "the use of information and communication technologies to deliver healthcare when patients and care providers are not in the same physical location".
- On this page you can find information on telehealth through webinars, case studies, resources and research.

There are 3 key areas within the broader telehealth space that are currently being developed: telemedicine, telemonitoring and mHealth (mobile health).
- Telemedicine is "the use of telecommunication and information technologies in order to provide clinical health care at a distance". Within New Zealand, the most common types of telemedicine are Video conferencing and Store and forward. You can read more about each of these at NZ Telehealth Resource Centre.(external link)
- Telemonitoring refers to "remotely collecting and sending patient data so that it can be interpreted and then contribute to the patient's ongoing management". One of the big advantages of telemonitoring is enabling patients to be at home or their usual place of residence, such as an aged care facility, while their healthcare team can monitor vitals such as blood pressure, heart rate or activity levels. It can also be used for alarm systems, such as fall detection and treatment adherence.
- Telemetry takes this a step further and refers to collecting and sending data, such as heart rhythm monitoring, in real time.
- mHealth (also known as mobile health) describes "the use of mobile communications technologies in medical and public health practice, including the delivery of health information, health services and healthy lifestyle support programmes" (NZ Telehealth Resource Centre). A number of devices can be used to deliver mHealth, ranging from smartphones to tablets and mobile sensors. Mobile communications technology enables additional functionality to be used, such as text messaging (SMS), mobile apps, mobile web browsing, video calling, MMS/pxt, QR code scanning and GPS location. The portability and popularity of mobile devices is obviously a major advantage and newer technologies will keep appearing as technology advances.
Data type: The type of data you use might be standalone video or audio, combined video and audio, text (eg, blood pressure, weight and symptoms), continuous monitoring streams, alarm signals or specialised recordings (eg, ECG and EEG).
Data transfer: Data transfer can take place in real-time (synchronous), where the patient is usually present, or on a store and forward basis (asynchronous), where the patient is not usually present.
Who it involves: Clinicians and patients, and patients’ family and whānau, are the main parties usually involved in a telehealth consultation. It is possible for a number of people to take part in video conferences. For example, a consultant might be with a medical student at one site, while a patient, members of their whānau and a rural nurse specialist are at another site.
The type of consultation: A number of different types of consultations can take place using telehealth. These include:
- initial specialist assessment
- follow-up appointments
- discharge planning meetings
- multidisciplinary team meetings
- acute assessments
- ward round
- triage assessments
- therapy/treatment appointments.
Scheduling the consultation: Planned consultations are usually scheduled ahead of time, with locations and equipment booked by both parties. Facilities likely to need to have urgent consultations, such as emergency departments, can quickly make the appropriate equipment available.
A telehealth tips sheet for members by members(external link) was created by the RNZCGP in 2022.
- For patients: Faster access to care and shorter wait times. Remote patients can remain close to home, making consultations more convenient and reducing travel.
- DHBs: Fairer health system because of better access to care. More educational options for DHB staff via specialist video training.
- Specialists/consultants: Less time spent travelling for consultations. Greater control over scheduling. Closer working relationship between specialists and primary care.
- Aged care workers/nurses: Reduced need to transfer to older patients. Increased nurses' knowledge through more exposure to specialist consultations.
- General practitioners: GPs who serve rural health facilities need to travel less frequently. Store and forward allows for accessible referrals and second opinions.
- Allied health workers: Rehabilitation and physiotherapy can take place via video conference, meaning less time and budget spent on travel.
OpenNotes is the term given to opening up the health record so that patients can see their own notes and medical record including consultation records, lab results, immunisations, medications and recalls. This is done through the patient portals.
There are numerous benefits for patients and their healthcare providers. Read more about OpenNotes.
| AI and telehealth (external link)(NZ Telehealth, 2023) A panel of expert speakers explore the intersections of AI and telehealth and its potential to enhance patient care, improve diagnostics and expand access to medical services. They also delve into the challenges AI brings, eg, evaluation and regulation, privacy, accountability and much more. Panel: Chris Paton, Mike Mulvaney, Tania Moerenhout, Liam Caffery and Robyn Whittaker |
|
|
When the microphone is on(external link) (NZ Telehealth, 2023) |
|
|
Telehealth Success Stories from Aotearoa(external link) (NZ Telehealth, 2022) |
|
| Western Australian Telehealth Command Centre(external link) (NZ Telehealth, 2022) Learn about the 6 functions of the Command Centre, its origins and implementation, the benefits for patients and the community, and learnings from Medical Director – Dr Justin Yeung and the team from the WACHS Command Centre. Panel: Dr Justin Yeung, Dr Aled Williams, Dr Amanda Villis, Dr Adnan Afridi, Mel Goode and Sallie Walsh |
|
| Telehealth Apps Webinar - Innovative Inclusion for Aotearoa(external link) (NZ Telehealth, 2022) An insightful webinar where moderators Sarndrah Horsfall and Karen Ellis introduce panellists (several of the healthcare providers who have received support from the Digital Enablement Programme) who present and actively discuss their telehealth apps including: Tuku Iho, Digi Language Support (DLS), and Rapid Rehita. Panel: Fay Selby-Law, Kelly Feng, Dr Bo Ning, Tom Mclean, Theresa Mclean |
|
| Goodbye Postcode Lottery – Hello PASE(external link) (NZ Telehealth, 2022) A webinar actively discussing the benefits, enablers, and barriers of PASE. The system is a centralised telehealth model of care with a nationwide rostering system for specialist doctors, GPs, nurses and health workers, delivering timely care to patients no matter where they live. Panel: Dr Ruth Large, Andrew Morgan, Sarah Dalton, Megan Tunks, Joanne Doherty and Natalia Zuleta |
|
| Achieving Pae Ora(external link) (NZ Telehealth, 2022) Pae Ora (Healthy Futures) is the Government’s vision for Māori health. It provides a platform for Māori to live with good health and wellbeing in an environment that supports a good quality of life. The Pae Ora bill provides for a new structure and new accountability arrangements for the publicly-funded health system, in order to protect, promote, and improve the health of all New Zealanders. Panel: Erena Wikaire, Sasha Webb and Bernard Te Paa |
|
| Lessons Learnt and Highlights – Community Telehealth Initiatives(external link) (NZ Telehealth, 2022) A great line-up of panellists talk about their own experiences in telehealth, and share their learnings, including what’s working and what’s not, along with their highlights and lessons learnt along the way. Panel: Jen Coatsworth, Ani Olson, Sue Westbrook, Amio Matenga and Malcolm Kendall |
|
 |
Zoom Fatigue 'take two'(external link) (NZ Telehealth, 2022) An insightful webinar where panellists share experiences and identify and explore practical ways to overcome fatigue, the impacts of burnout, as well the psychological aspects of being on screen. Panel: Alex Kemp, Dr Rachel Webb, Miriam Wood |
 |
Disability and Telehealth 'take two'(external link) (NZ Telehealth, 2022) Panellists address access needs, and engagement for disabled people in telehealth. Hear different perspectives where panellists share experiences, explore the benefits of telehealth for providers and disabled people, and identify difficulties when accessing telehealth services. Panel: Mary Schnackenberg, Sue Emirali, Annette Rotherham, Dr Sally Britnell |
 |
Introduction to telehealth in cancer care(external link) (NZ Telehealth, 2022) This webinar focuses on how telehealth is currently being used in public, private and community cancer care settings and a new breast cancer telemonitoring pilot. There will also be discussion on what changes are needed to better support cancer clinicians using telehealth. Panel: Adele Gautier, Elinor Millar, Iain Ward, Jo Stafford, Marie Wales |
 |
What does telehealth look like in 2022 for primary care(external link) (NZ Telehealth, 2022) The first telehealth webinar of 2022 kicks off with a special webinar brought to you in collaboration with Aotearoa Collaborative. Panellists will talk to their own experiences in primary care, including telehealth in oncology and palliative care, patient portals and the importance of video consultations in a Omicron COVID-19 world. Panel: Jess White, Dr Janine Bycroft, Dr Jeff Lowe, Angela Blunt, Tania Kemp |
 |
New and emerging healthcare innovation(external link) (NZ Telehealth, 2021) Our line-up of panellists talk to their own experiences in primary care, including telehealth in oncology and palliative care, patient portals and the importance of video consultations in a Omicron COVID-19 world. Panel: Josh Robb, Dr Richard Medlicott, Patrick Salmon, Dr Steve Earnshaw, Jon Herries, Dr Robyn Whittaker, Dr Emily Gill |
 |
Telemonitoring(external link) (NZ Telehealth, 2021) This month’s webinar explores telemonitoring and marks the launch of the National Remote Patient Monitoring guidelines developed from experience and guidance from members of the Virtual Health Industry Group (VHIG) within the NZ Health IT (NZHIT) cluster, in collaboration with the New Zealand Telehealth Leadership Group (NZTLG). Panel: Christopher Dawson, Kathryn O’Neill, Mark Smith, Philip Jones, Jeremy Morris |
 |
Improving Maori health gains(external link) (NZ Telehealth, 2021) Digital enablement tools are used daily in Aotearoa to support and improve Maori hauora. This webinar delves into virtual services who navigate to engage and serve Maori, Pacific and other communities with unmet needs. Panel: Sasha Webb, Jade Chase, Dr Mataroria Lyndon, Dr Lily Fraser, Bernard Te Paa |
 |
Improving Maori health gains(external link) (NZ Telehealth, 2021) Panellists address telehealth access in the disability community, share experiences, explore the benefits of telehealth for providers and people with disabilities, identify difficulties that people with disability face when accessing telehealth services, discuss resources available and maintaining accessible services. Panel: Prudence Walker, Mary Schnackenberg, Sue Emirali, Brooke Dibley |
 |
Telehealth Providers(external link) (NZ Telehealth, 2021) This webinar showcases New Zealand telehealth public providers and features a great line-up of panellists from Emergency Consult, Well Revolution, Tend and CareHQ. Panel: Prudence Walker, Mary Schnackenberg, Sue Emirali, Brooke Dibley |
 |
Telehealth Mental Health(external link) (NZ Telehealth, 2021) The panelists presents some of their projects and reveal insights on a telehealth approach for assessing and addressing those with mental health issues, and how this can build capacity to support the youth and the elderly, and beyond. Panel: Dr. Siale Foliaki, Dr. David Codyre, Dr. Lyndy Matthews, Dr. Janine Bycroft |
 |
Telehealth International Leaders(external link) (NZ Telehealth, 2021) This webinar extends beyond the New Zealand border to learn about telehealth on an international scale. With panellists from Scotland and Australia, this is an interesting discussion exploring three key themes and how they have fundamentally changed the future of the healthcare industry. Panel: (Scotland) Margaret Whoriskey, Nessa Barrt, Morag Hearty (Australia) Nicole Bate, Kate Hawkings |
 |
Telehealth in Primary & Community Settings(external link) (NZ Telehealth, 2021) This webinar aims to share experience of those already familiar with telehealth and provide core information to those with an appetite for it. It highlights the positive steps, as well as address the remaining challenges including how to decrease risk, the importance of a trusting relationship between patient and clinician, and ideas for continued improvement. Panel: Ruth Large, Megan Tahere, Linzi Birmingham, Billy Allan |
 |
Back to Basics(external link) (NZ Telehealth, 2021) The webinar will be an opportunity to hear about experiences from a line-up of panellists from different health sector backgrounds and support those who are new to telehealth or would like to revisit core information. Panel: Ruth Large, Megan Tahere, Linzi Birmingham, Billy Allan |
 |
What I Learnt in 2020(external link) (NZ Telehealth, 2020) This is the last telehealth webinar of the year and features a line-up of panellists who will reflect on telehealth in 2020 and celebrate the huge strides in telehealth in New Zealand. Panel: Dr Janine Bycroft, Amio Ikihele, Yariv Doron |
 |
Equity & Improving Access with Telehealth(external link) (NZ Telehealth, 2020) Covid-19 has triggered rapid changes in the delivery of health services, and highlighted the need to address equity by improving access. The use of telehealth solutions can assist providers in providing continuity of care in a safe, secure and sustainable way. Panel: Dr Nina Scott, Lily Fraser, Amio Ikihele, Dr Leanne Te Karu, Prudence Walker, Dr Wiki Gillespie |
 |
Allied Health(external link) (NZ Telehealth, 2020) Moderated by Rebecca George, this webinar focusses on telehealth adoption in allied health. This specialised topic features panellists who will share their experiences and thoughts on the benefits and challenges for continued high-quality care. Panel: Pip Zammit, Sharon Russell, Miranda Buhler, Aoife O’Reilly, Aimee Dackers |
 |
And then COVID-19 happened... an update on the national Health Information Platform(external link) (NZ Telehealth, 2020) On 2 September 2019, Cabinet approved the development of a business case for the national Health Information Platform to improve access to and use of health information as a key enabler of an eective and sustainable health and disability system. The Ministry engaged with the sector and other agencies to develop a programme business case that was scheduled for Cabinet review in March 2020. |
 |
Scotland Telehealth(external link) (NZ Telehealth, 2020) Moderated by Dr Ruth Large, a panel of experts from Scotland share their experiences and thoughts on how telehealth is being implemented in Scotland and what benefits and challenges they are experiencing in primary and secondary healthcare. Panel: Nessa Barry, Morag Hearty |
 |
Using telehealth for cancer care during COVID-19(external link) (NZ Telehealth, 2020) This webinar reflects on the use of telehealth during COVID-19 and promote its use in the future. A range of experts will share their experiences and thoughts on the benefits and challenges for continued high-quality care. Panel: Dr Claire Hardie, Michelle Mako, Dr Richard Isaacs, Marie Wales, Anne Fraser |
 |
Health literacy - getting the most from telehealth(external link) (NZ Telehealth, 2020) This webinar provides techniques to ensure you get the information you need in a telehealth environment, and that consumers get the information and assistance they need from a consult to take appropriate and timely action. These will reflect some of the ways you already work in-person, adapted to work across telehealth platforms, as well as offering some new approaches. Panel: Dr Janine Bycroft, Carla White, Susan Reid, Dr Martin Mikaere |
 |
NZ Regulation and Legislation for Telehealth(external link) (NZ Telehealth, 2020) In this webinar, we start to explore the regulation and legislation relevant to telehealth in New Zealand. Guests will discuss a broad range of topics including privacy, consent, medicolegal, prescribing and many more topics. Panel: Dr Ruth Large, Dr Sam Murton, Rommel Anthony, Diana Aquiliana, Dr Samantha King |
 |
Telehealth TECH Security, privacy, software and hardware(external link) (NZ Telehealth, 2020) This webinar explores the very big topic of what technology solutions are available to use for telehealth. Although the webinar will touch on the use of phone, it will focus mainly on video, and video consultations. |
 |
Introduction to telehealth in NZ (external link)(NZ Telehealth, 2020) This webinar assists providers in achieving safe, secure and sustainable telehealth solutions which complement their existing in-person relationships. Panel: Dr Samantha Murton, Dr Jon Bonning, Rebecca George, Dr Samantha King, Amio Ikehele |
 |
NZ telehealth update from Dr Ruth Large(external link) (external link)(NZ Telehealth, 2020) |
On this page, you can find the following information:
- DHBs increase use of telehealth for clinical care
- Telehealth links rural hospitals to ICU
- Bill's telehealth story
- Nelson Marlborough telehealth video
DHBs increase use of telehealth for clinical care
The following information is taken from eHealthNews.nz(external link).
A “promising” new telehealth report shows a significant increase in the number of providers and services using telehealth for the delivery of clinical care.
However, ongoing barriers to uptake and silos of data and knowledge around telehealth means successful pilots have not always translated into business as usual services.
The 2019 Telehealth Survey updates one published four years ago and shows uptake has increased considerably across all 20 district health boards, with more than 1300 telehealth initiatives either active, in pilot or planned.
“Many organisations are turning to telehealth as they strive to improve the services they deliver,” the report says.
“However, uptake of telehealth often relies on local champions and although many barriers have improved (namely interconnectivity and cost) barriers such as lack of clear leadership and governance, difficulty circumnavigating funding models and access to devices and high-speed internet connections remain.”
Read more: DHBs increase use of telehealth for clinical care(external link).
See also the following articles on telehealth in New Zealand:
Telehealth on the rise(external link)
Telehealth gets $20 million injection(external link)
Telehealth resources support uptake of virtual care(external link)
Telehealth links rural hospitals to ICU
The following information is taken from the Northland DHB website(external link).

Whangarei ICU's Dr Michael Whangarei ICU’s Dr Michael Kalkoff discusses a recent case with Kaitaia Hospital Senior Medical Officer Damian Marsh and Registered Nurse John Walker via RITA. Image credit: Northland DHB(external link)
Northland District Health Board has developed a new mobile telehealth cart and linked all of its rural hospitals (Kaitaia, Bay of Islands, Dargaville and, in 2020, Rawene) to the intensive care unit at Whangārei Hospital.
The Northland telehealth and mobility team developed this cart in conjunction with Northland DHB intensive care physicians, Connect NZ, healthAlliance and the University of Queensland Centre for Online Health.
The carts allow remote patient assessment and management in the acute clinical setting, enhance assistance and decision making for acute retrieval requests from rural hospitals, and provide Whangārei Hospital with an after-hours telestroke service.
The acute retrieval service is called RITA or Rapid Information Telehealth Assessment and uses Zoom videoconferencing from a computer workstation, tablet or cell phone enabling a much broader and more integrated communication network than previously.
The mobile carts are moved to the patient’s bedside and from there all other functionality is controlled at the ICU end, enabling rural hospital teams to be hands off with the technology and concentrate on their patient. The ICU end can control the call and functions of the two cameras. The second camera has a powerful zoom, which is also remotely controlled.
RITA enhances Whangārei ICU’s remote acute assessment capabilities to rural hospital emergency departments and wards, patient safety through direct rapid patient assessment, as well as advising on patient management of the acutely unwell patient. This includes assisting with decision-making in determining the safest way to transport the patient.
Read more: Telehealth linking rural hospitals to ICU(external link).
Bill's telehealth story
(Nelson Marlborough Health, NZ, 2021)
The Waikato DHB renal service covers the Waikato area but also from coast to coast all the way from Raglan on the west coast all the way to Gisborne on the east coast. A video conference solution is reducing the burden of travel for patients and providing more timely access to specialists.
Telehealth renal case study
(Mobile Health, NZ, 2017)
Nelson Marlborough telehealth video
Nelson Marlborough Health is aiming to increase the use of Virtual health clinic clinical consultations to avoid the stress and travel for patients associated with attending appointments in person.
Some clinicians talk about their experiences using telehealth.
(Nelson Marlborough Health, 2020)
NZ Telehealth Forum & Resource Centre
Resources to support the implementation of video and phone consultations are being collated on the NZ Telehealth Forum & Resource Centre website(external link).
Key sections include:
- Health providers(external link)
- Questions about security(external link)
- Software(external link)
- Hardware(external link)
- Implementation(external link)
- Technology(external link)
Additional resources for GP clinics are available on the Healthcare Home Collaborative website(external link) including:
- Video consultations toolkit – download PDF(external link)
- Telephone triage – download PowerPoint(external link)
- Patient portal – download PowerPoint(external link)
Telehealth clinical modules ProCare, NZ, 2022
Abdominal assessment (external link)
Dermatology(external link)
Mental health(external link)
Musculoskeletal assessment(external link)
Pregnancy care(external link)
Respiratory assessment(external link)
Other resources
- Telehealth tips sheet for members by members(external link) RNCGP, NZ, 2022
- Specialist GP telehealth consultations position statement [PDF, 189 KB] RNZCGP, NZ, 2022
- New Zealand telehealth survey report 2019(external link) NZ Telehealth, 2019
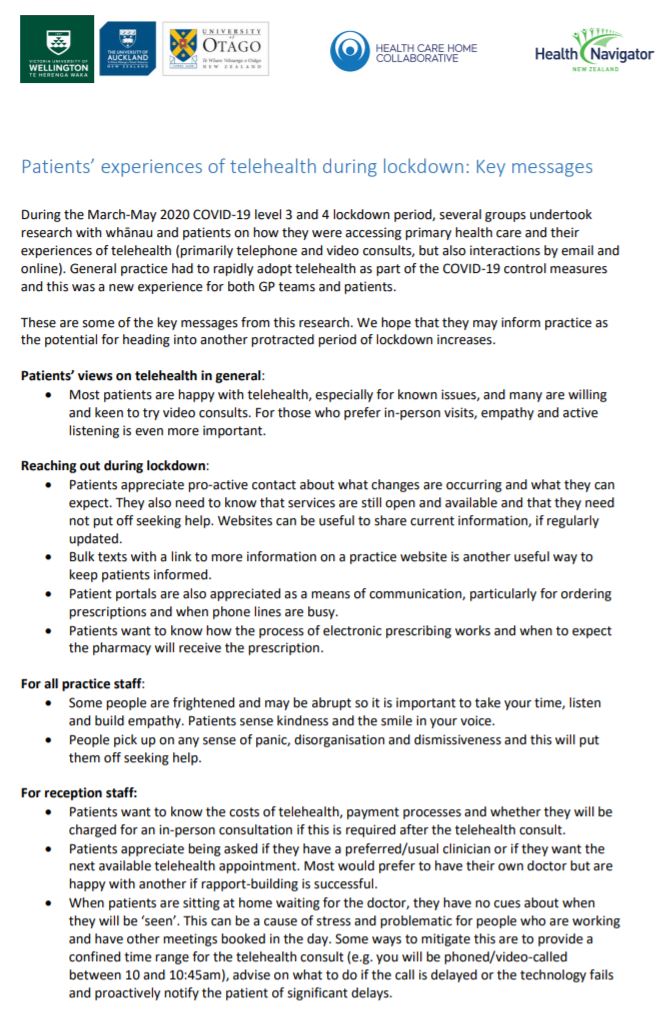
- Patients’ experiences of telehealth during lockdown [PDF, 195 KB] Victoria University of Wellington, University of Auckland, University of Otago, Healthify He Puna Waiora, NZ and Health Care Home Collaborative, NZ, 2020
- Healthcare Home – GP Guide(external link)
- Patients’ experiences of telehealth during lockdown [PDF, 195 KB]Victoria University of Wellington, University of Auckland, University of Otago, Health Care Home Collaborative & Healthify He Puna Waiora, NZ
- Telemedicine and preventative health podcast(external link) Goodfellow Podcast, NZ, 2020
- Providing support by phone or video call(external link) Te Pou, NZ
- Ten tips for assessing patients for COVID-19 during a telephone consultation(external link) COVID-19 BPAC Bulletin, NZ
- Allied health best practice guide for telehealth(external link) Allied Health Aotearoa New Zealand
- Guidelines for the use of telepsychology in treatment of ACC clients(external link) ACC, NZ
- Teletherapy policy(external link) Safe Network NZ
- New Zealand telehealth survey report 2019(external link) District Health Boards
- Telehealth (Digital Practice) handbook – a practical guide for physiotherapy Southern DHB, NZ, 2020
- Strategic review of telehealth in NSW – final report(external link) NSW Ministry of Health, Australia
- Telehealth framework and implementation strategy 2016–2021(external link) NSW Ministry of Health, Australia
- Telehealth in practice guide(external link) NSW Ministry of Health, Australia
- Can telerehabilitation replace traditional care webinar(external link) Duke University, UK
| Resources |
|
Effect of telehealth extended care for maintenance of weight loss in rural US communities
|
|
Managing patients with chronic pain during the COVID-19 outbreak: considerations for the rapid introduction of remotely supported (eHealth) pain management services
|
|
The effect of augmented speech-language therapy delivered by telerehabilitation on poststroke aphasia – a pilot randomized controlled trial
|
|
Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19)
|
|
Digitally enabled aged care and neurological rehabilitation to enhance outcomes with Activity and MObility UsiNg Technology (AMOUNT) in Australia: A randomised controlled trial
|
|
Digital transformation in the era of COVID-19: Health Informatics NZ (HiNZ) webinar
|
|
The benefits, challenges and learnings of telehealth in rehabilitation practice: NZ Rehabilitation Association webinar
|
Learn more
Video consulting: Not just a consultation plus tech(external link) BJGP LIFE
Statement on use of the internet and electronic communication(external link) Medical Council of New Zealand
Telehealth March 2020(external link) Medical Council of New Zealand
Telehealth prescribing in NZ(external link) NZ Telehealth Forum & Resource Centre
Providers(external link) NZ Telehealth Forum & Resource Centre
Standards(external link) NZ Telehealth Forum & Resource Centre
Telecommunications information privacy code 2003(external link) Privacy Commissioner, NZ
Guide to providing telephone and video consultations in general practice(external link) Royal Australian College of General Practitioners
Telephone and video consultations in general practice: Flowcharts(external link) Royal Australian College of General Practitioners
Virtual consultations(external link) Royal New Zealand College of General Practitioners
Telehealth for global emergencies: COVID-19(external link) The University of Queensland Centre for Online Health, Australia
Clinical images(external link) Auckland Regional HealthPathways
Clinical images and the use of personal mobile devices – a guide for medical students and doctors(external link) NZMA
Reference
- COVID-19 telehealth(external link) Canterbury Community HealthPathways, NZ, 2020
Brochures
NZ Telehealth, 2019
Victoria University of Wellington, University of Auckland, University of Otago, Healthify He Puna Waiora, NZ and Health Care Home Collaborative, NZ, 2020
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Page last updated:



