- Bartholin’s glands are a pair of pea-sized glands found in the vulva either side of the opening to the vagina. They secrete fluid that acts as a lubricant during sex.
- If the duct (opening) from the glands becomes blocked, they can fill with fluid and expand to form a soft, painless lump or cyst, known as a Bartholin’s cyst.
- It doesn't usually cause any problems, but if it grows larger it may become uncomfortable during sex.
- It can also become infected, and form an abscess. If this happens, you may notice redness and feel pain in the area when you walk, sit down or have sex.
- Treatment depends on the size of the cyst, how painful it is and whether it is infected or not.
- Around 1 in every 50 women will develop a Bartholin’s cyst or abscess. It is most common in sexually active women aged between 20 and 30.
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Bartholin’s cyst
Also called a Bartholin’s duct cyst
Key points about Bartholin's cysts
- A Bartholin’s cyst is a lump that forms in the opening to your vagina when the Bartholin’s gland openings get blocked.
- The cyst is soft and painless and doesn’t generally cause any problems.
- If it gets larger or infected it can cause pain when walking, sitting or during sex.
- If you find a lump near or in your vagina, always get it checked by a healthcare provider.

About 2% of women will develop a Bartholin’s duct cyst or abscess at some point in their life (abscesses are more common than cysts). It's usually not known why Bartholin’s ducts become blocked, but once a lump (cyst) has developed, the fluid inside can easily become infected. Usually, the infection is from bacteria commonly found in the vagina. However, sometimes bacteria that can cause sexually transmitted infections (eg, gonorrhoea or chlamydia) cause the infection.
The image shows a Bartholin's cyst on the edge of the vagina.
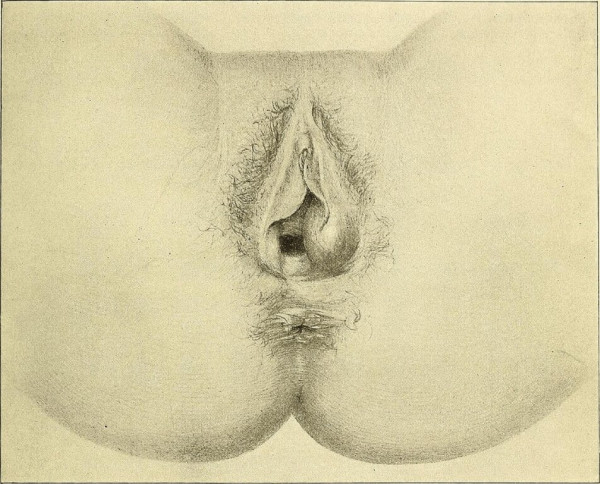
Image credit: Internet Archive Book Images via Wikimedia Commons
You might feel a lump near your vaginal opening. This is usually painless but it can be tender. If the cyst becomes infected, you may experience:
- a tender, painful lump near your vaginal opening
- discomfort while walking or sitting
- pain during intercourse.
Always see your healthcare provider if you find a lump near your vagina so they can confirm a diagnosis and ensure you get appropriate treatment. If your healthcare provider thinks the cyst may be infected, they may swab it and send a sample to the lab for analysis to identify the bacteria responsible. In some cases, it may be recommended you have a biopsy (sample of tissue removed) so it can be checked for signs of a rare cancer, called Bartholin’s gland cancer.
Depending on the size of the cyst or abscess, and the severity of your symptoms, treatment options range from self-care and medication to drainage or surgical removal of the cyst.
Self-care
If you can feel the cyst, but it’s not growing, sore or infected, it's unlikely you’ll need any treatment. If the cyst is painful, your healthcare provider may recommend some simple self-care measures such as:
- soaking the cyst in warm water several times a day for 3 or 4 days using a sitz bath or using warm compresses on the area
- taking over-the-counter painkillers, eg, paracetamol or ibuprofen
- taking the full course of antibiotics if they’ve been prescribed for you.
Medicine
If the cyst is infected (developed into an abscess), and you’re becoming more unwell, your healthcare provider may prescribe antibiotics. If the cyst or abscess is bothering you or keeps coming back, you may need to have one of the following procedures.
Word catheter balloon insertion (procedure)
This procedure takes around 15 minutes and is carried out under a local anaesthetic. It involves making a channel from the cyst or abscess to your vagina, so the gland can drain. A small cut is made in the abscess and a small flexible tube (catheter) with a small balloon at its tip is inserted to create a passage. It is usually offered to women under 40 years of age. The catheter is usually left in for a few weeks, to allow the tract to form properly and make sure drainage will continue once the catheter is removed.
Marsupialisation (surgery)
This surgery is done under general anaesthetic and takes about 10 to 15 minutes. The doctor makes a small cut in the abscess and gland to release the fluid, sewing the edges of the cyst/abscess to the surrounding skin. This keeps the cyst t open, so it can heal and allow the fluid to drain out. The small cut will completely heal by itself.
Excision (surgery)
This surgery involves the removal of the cyst or abscess under general anaesthetic. It’s carried out so that the area can be fully examined when the cyst or abscess is removed. During excision, the entire gland is removed. This procedure is only considered in women over 40 who’ve had abscesses recur (come back) on several occasions. As result of excision, the gland will no longer function which means that your body will produce less lubricant.
This loss of lubrication can make having sex uncomfortable. To improve lubrication, you can use lubricants or vaginal moisturisers. If these are not effective for you, talk to your healthcare provider about whether vaginal oestrogen and hormone replacement therapy (HRT) are suitable for you.
How can I prevent a Bartholin’s cyst?
Because it's not clear exactly why Bartholin's cysts develop, it isn't usually possible to prevent them. However, some cysts are thought to be linked to sexually transmitted infections, so practising safe sex (using a condom every time you have sex) might help reduce your chances of developing one.
Unfortunately, Bartholin’s cyst/abscesses can come back, even after treatment with a word catheter or marsupialisation.
The following links provide further information about Bartholin’s cyst. Be aware that websites from other countries may have information that differs from New Zealand recommendations.
Bartholin's cyst and abscess(external link) Patient Info, UK, 2017
Bartholin’s cyst(external link) NHS, UK, 2015
Sitz bath(external link) Healthline, US, 2017
Treating a Bartholin's cyst or abscess [PDF, 96 KB] Guys’ and St Thomas’ NHS Foundation Trust, UK, 2017
References
- Haider Z, Condous G, Kirk E, Mukri F, Bourne T. The simple outpatient management of Bartholin's abscess using the Word catheter – a preliminary study(external link) Aust N Z J Obstet Gynaecol. 47 (2): 137–140.
- Treating a Bartholin's cyst or abscess [PDF, 96 KB] Guys’ and St Thomas’ NHS Foundation Trust, UK, 2017
- Bartholin's cyst(external link) Mayo Clinic, US, 2015
- Vaginal dryness(external link) NHS Choices, UK, 2016
- Bartholin’s cyst(external link) Auckland HealthPathways, NZ, 2019
Although incision and drainage is the most frequently performed procedure, it is associated with a high rate of recurrence. Oral antibiotics are not indicated unless there is associated cellulitis or systemic symptoms. If required, broad-spectrum antibiotic cover is necessary as the infection is usually polymicrobial. Carcinoma of the Bartholin gland is rare (approximately 1% of genital malignancies in women), however, this diagnosis should be considered in a woman aged over 40 years. Vulvovaginal health in premenopausal women(external link) BPAC, NZ, 2011
Because the Bartholin's glands usually shrink during menopause, a vulvar growth in a postmenopausal woman should be evaluated for malignancy, especially if the mass is irregular, nodular, and persistently indurated. Omole F, Simmons BJ, Hacker Y. Management of Bartholin's duct cyst and gland abscess(external link) Am Fam Physician. 2003 Jul 1;68(1):135-140.
Bartholin's cyst(external link) BMJ Best Practice, UK, 2017
Credits: Healthify editorial team. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Dr Phoebe Hunt, Medical Officer, Northland
Last reviewed:





