| Opioid overdose is an emergency and must be treated immediately. Call 111 for help if you suspect someone has overdosed on opioids. |
Low or no data? Visit zero.govt.nz, scroll down the page then click on our logo to return to our site and browse for free.
Opioid overdose
Key points about opioid overdose
- Anyone using prescribed or street opioids can have an overdose.
- Opioids affect the part of your brain that controls your breathing.
- When you take more opioids than your body can handle (overdose), your breathing slows. It can cause death in a worse case event.

Opioids are medicines commonly used to treat pain. Examples of opioids include codeine, morphine, oxycodone, methadone, fentanyl, tramadol and buprenorphine. Opioids can also be so-called street drugs, such as heroin.
Anyone using prescribed or street opioids can have an overdose, but there are some things that put you at higher risk.
You are at risk of an opioid overdose if you are taking prescription opioids more often or at higher doses than recommended, or if you are taking opioids with alcohol or other medicines such as benzodiazepines (sleeping tablets).
An overdose can also happen if you misuse opioids. For example, extended-release opioid tablets are meant to be swallowed whole. If you crush or break these pills before taking them, it may cause an overdose because too much of the drug is released at once.
Injecting drugs and using drugs of unknown purity or strength can also increase your risk of opioid overdose. Opioids that are available on the street are of unknown strength and type and so their effects can vary.
Having other health conditions, like liver or kidney disease or breathing problems, increases your risk of opioid overdose.
A person may have opioid overdose if they:
- are very sleepy or hard to wake up (passed out)
- have irregular, little or no breathing
- are snoring unusually or deeply
- are making gurgling sounds
- have blue lips or nails
- limp and floppy
- vomit
- have tiny pupils.
It can cause death in a worst case event.

Image credit: Opioid overdose family support toolkit(external link) Ohio State University, US
| Opioid overdose is an emergency. Call 111 for help if you suspect someone has overdosed on opioids. |
|
While you are waiting for help:
|
Naloxone emergency kit
Opioid overdose is treated with the medicine naloxone. If taken soon enough after an opioid overdose, it can reverse the effects of opioids and save lives. If you are at risk of opioid overdose you can be prescribed a naloxone emergency kit for use in an emergency. If you have access to naloxone read about how to administer naloxone in an emergency.
Reduce the risk
If you use opioids, you can reduce your risk of overdose or death by:
- not using when you are by yourself
- knowing your tolerance (how much you can take)
- having a naloxone kit available, and knowing how to use it
- using a small amount of an opioid first to check the strength
- not taking opioids with alcohol or other drugs (unless prescribed by your doctor).
| If you are taking opioids for pain |
|
‘Start low, go slow’ If you have been prescribed an opioid start on a low dose and increase slowly as your doctor has prescribed it. Do not exceed the prescribed dose. Different formulations (eg, tablet, capsule, patch) will suit different people. Do not take someone else's opioid medicine. Set a goal Set a goal for treatment. It should not just be about pain reduction but also a focus on returning back to activities such as exercise or work. When to reduce or stop taking opioids Have an agreement in place in advance on when to start reducing or stopping an opioid. This is known as tapering.
Harm can include developing a dependence (physical, psychological or both), opioid-induced hyperalgesia, and tolerance or withdrawal. Read more about lowering opioid doses. Regular reviews See your GP regularly. They can help monitor the progress of treatment. If the benefits of taking opioids are outweighed by the potential harm, there are other options for treatments. These include non-opioid medicines and non-medicine treatments such as physiotherapy and acupuncture. Read more about non-medicine treatments for pain. |
Read more about medicines and side effects and reporting a reaction you think might be a side effect.
- Opioids information video(external link) NPS Medicinewise, AUS
- Maximising opioid safety(external link) Monash University, AUS
- Opioid medicines and chronic non-cancer pain (external link) NPS Medicinewise, AUS
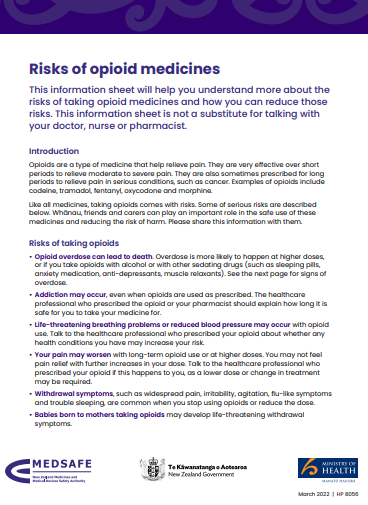
- Risks of opioid medicines(external link) Medsafe, NZ
Resources
Risks of opioid medicines(external link) Medsafe, NZ, 2022
5 questions to ask about your medications(external link) Health Quality and Safety Commission, NZ, 2019 English(external link), te reo Māori(external link)
References
- Take-home naloxone in Australian hospitals(external link) SHPA, AUS
- Opioid overdose(external link) World Health Organization
Brochures
Medicines and side effects
Healthify He Puna Waiora, NZ, 2024
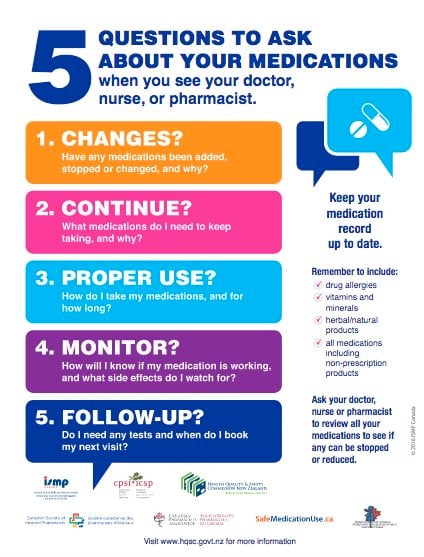
Health Quality and Safety Commission, NZ, 2019 English, te reo Māori
Credits: Maya Patel, Pharmacist, Auckland, Pharmacist, Healthify He Puna Waiora. Healthify is brought to you by Health Navigator Charitable Trust.
Reviewed by: Sandra Ponen, Pharmacist
Last reviewed:
Page last updated:





